Combined Spinal-Epidural Anesthesia?
Preface
Origin
Soresi technique
Curelaru technique
Needle-through-needle technique
Eldor needle technique
Huber needle technique
Eldor, Coombs and Torrieri technique
Indications
Problems
The twin theory
Failed spinal or epidural anesthesia
One needle technique for combined spinal-epidural
anesthesia
Aspiration pneumonia prevention by the CSEA
Intraoperative challenges
Anesthesia and public image
Huber needle and Tuohy catheter
Total spinal anesthesia: The origin of CSEGA
What is anethesia?
Use of ephedrine in CSEGA
Cardiovascular effects of CSEGA
Cord ischemia and preemptive analgesia
CSEA for Cesarean section
Corning
Bier
A new look at the lumbar extradural space pressure
Do not rotate the epidural needle
Epidural rostal augmentation of spinal anesthesia
Metallic particles in the needle-through-needle
technique
Superselective spinal anesthesia
CSEA in uncommon disease
CSEA for laparoscopic operations
Postoperative epidural analgesia
Unilateral spinal anesthesia
CSEA for abdominal operations
CSEA for thoracic operations
Anesthetic risk factors
Medico-legal aspects of CSEA
Spinal opioid pruritus and emesis
Endocrine responses to spinal or epidural anesthesia
Epidural unilateral blockade
Combined spinal-epidural anesthesia: The anesthesia
of choice
Epidural catheter strength
Epidural catheter paresthesias
CSEA and anticoagulation
Combined spinal-epidural analgesia in labor
Combined spinal-epidural anesthesia for orthopedic
operations
Combined end-multiple lateral holes (CEMLH) epidural
catheter
Double-hole pencil-point spinal needle
Epidural catheter test dose in the combined spinal-epidural
anesthesia
Spinal and epidural opioid analgesia
The choice of the anesthesiologists
Epidural catheter malposition
Woolley and Roe case
Anesthetic costs
From the skin to the spinal-epidural spaces
Myint case
Spinal needles
Meningitis post spinal-epidural anesthesia
Preemptive analgesia and combined spinal-epidural
anesthesia
Sympathetic innervation and CSEA
The politics of anesthesiology
Preconclusion
Conclusion
Preface
CSEA (combined spinal-epidural anesthesia) and CSEGA (combined spinal-epidural-general
anesthesia) are new modalities of anesthesia for almost any patient at
any age. This book highlights the subject from various points of view.
It doen`t intend to teach. It`s goal is to encourage the anesthesiologists
to practise what they already know in the best way they think is good for
themselves while being a patient. It is a kind of a balanced anesthesia
which uses techniques instead of drugs to accomplish the ideal kind of
anesthesia for the patients. This new frontier in anesthesia should open
a new era of anesthetic quality and cost-effectiveness. However, in the
second edition of Principles and Practice of Obstetric Analgesia and Anesthesia,
edited by Bonica JJ and McDonald JS, and published in 1995 by Williams
& Wilkins, there are 1344 pages. The chapter on epidural analgesia
and anesthesia contains 127 pages. That on subarachnoid block - 26 pages.
On subarachnoid/epidural combination there is only half a page with only
2 references in the chapter on cesarean section. So, the new combined spinal-epidural
anesthesia gained only 0.03% of the space in a book published in 1995 on
the practice of obstetric analgesia and anesthesia. This is really not
its present worth, neither its future...
"It has long been an axiom of mine that the little things are infinitely
the most important" (Arthur Conan Doyle).
"If pain could have cured us we should long ago have been saved"
(George Santayana).
"The greatest evil is physical pain" (St. Augustine of Hippo).
Origin
The first epidural analgesia was done by Corning (1) in 1885 inadvertently.
Lumbar dural puncture was introduced in 1891 by Wynter (2) in England and
Quincke (3) in Germany. Von Ziemssen (4) in 1894 suggested the feasibility
of injecting drugs by means of lumbar dural puncture. Bier (5), a surgeon
at the Royal Chirurgical Clinic in Kiel, was the first to inject cocaine
into the spinal space. It was between August 16 and 27, 1898. It took 52
years since Corning`s discovery of the epidural analgesia and 39 years
since Bier`s spinal anesthesia that these two compartments were first combined
by Soresi (6) in 1937. It took another 42 years until Curelaru (7) in 1979
used this combined spinal-epidural anesthesia again. Even the discoveries
of Corning and Bier are 13 years apart. However, the first anesthesia (maybe
it was combined spinal-epidural anesthesia - who knows?...) was done by
God (8) "caused a deep sleep to fall upon Adam" for rib extraction. The
combined approach can also have its origin in the Bible: "Two are better
than one" (9). Or you can look at it from Mark Twain`s point of view: "Name
the greatest of all the inventors. Accident". 1. Corning JL. Spinal anaesthesia
and local medication of the cord. NY Med J 1885;42:483-485 2. Wynter WE.
Lumbar puncture. Lancet 1891;1:981-982 3. Quincke HI. Die technik der lumbalpunktion.
Verh Dtsch Ges Inn Med 1891;10:321-331 4. Von Ziemssen HW. Allgemeine behandlung
der infektionskrankenheiten. Jena 1894 5. Bier A. Versuche uber Cocainisirung
des Ruckenmarkes. Dtsch Ztschr Chir 1899;51:361-369 6. Soresi AL. Episubdural
anesthesia. Anesth Analg 1937;16:306-310 7. Curelaru I. Long duration subarachnoid
anaesthesia with continuous epidural block. Praktische Anasthesie Wiederbelelung
und Intensivtherapie 1979;14:71-78 8. Genesis 2:21 9. Ecclesiastes 4:9
Soresi technique
Soresi (1) used a fine needle without stilet and introduced it into
the epidural space using the hanging drop technique. While in the epidural
space he injected 7-8 ml of dissolved novocain. Then he pierced the dura
and poured another 2 ml of dissolved novocain into the spinal space. This
gave his patients anesthesia for a period of 24-48 hours! He and his colleagues
employed this method in over 200 patients. He concluded that "by combining
the two methods many of the disadvantages of both methods are eliminated
and their advantages are enhanced to an almost incredible degree". 1. Soresi
AL. Episubdural anesthesia. Anesth Analg 1937;16:306-310
Curelaru technique
Forty two years later, the Swedish anesthesiologist, Curelaru (1), while
working in Bucharest, Romania, tested on 150 patients the method of spinal
anesthesia with continuous epidural block. The punctures of the epidural
and subarachnoid spaces were done through two intervertebral spaces. The
puncture of the epidural space was performed 1-2 intervertebral spaces
higher than the subarachnoid. Anesthesia was always started with the introduction
of an epidural catheter. After introducing the epidural catheter, the puncture
of the subarachnoid space was done, followed by subarachnoid injection
of the anesthetic solution. Curelaru concluded its advantages as "the possibility
of obtaining a high quality conduction anaesthesia, virtually unlimited
in time, the ability to extend over several anatomical regions the surgical
field, minimal toxicity, the absence of postoperative pulmonary complications
and the economy". 1. Curelaru I. Long duration subarachnoid anaesthesia
with continuous epidural block. Praktische Anasthesie Wiederbelelung und
Intensivtherapie 1979;14:71-78
Nedle-through-needle technique
Coates (1) from England and Mumtaz, Daz and Kuz (2) from Sweden, in
two separate letters in the same issue of Anaesthesia, in 1982, first described
the insertion of a long spinal needle through the epidural needle for performing
the combined spinal-epidural anesthesia. Coates found the technique "simple,
reliable and relatively quick to perform". After injecting the anesthetic
solution into the subarachnoid space, the spinal needle is withdrawn and
an epidural catheter is threaded through the same lumen of the epidural
needle, through which the spinal needle was inserted. 1. Coates MB. Combined
subarachnoid and epidural techniques. A single space technique for surgery
of the hip and lower limb. Anaesthesia 1982;37:89-90 2. Mumtaz MH, Daz
M, Kuz M. Combined subarachnoid and epidural techniques: Another single
space technique for orthopaedic surgery. Anaesthesia 1982;37:90
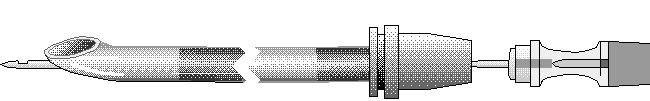
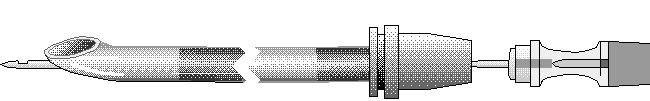
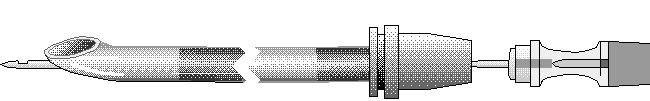
Eldor needle technique
The Eldor needle (1) was first described in 1990. The Eldor needle is
a combined spinal-epidural needle which is composed of an 18 gauge epidural
needle with a 20 gauge spinal conduit. This is a specialized needle for
the combined spinal-epidural anesthesia. There is no need of long spinal
needles. The epidural catheter can be inserted before the spinal anesthetic
injection. The Eldor needle facilitates the insertion of very small gauge
spinal needles through its spinal conduit, so significantly reduces the
incidence of post-dural puncture headache. There is no danger of epidural
catheter protrusion through the dural hole made by the spinal needle. There
are no metallic particles production while the spinal needle passes through
the bent epidural needle tip, as in the needle-through-needle technique.
The procedure of the Eldor needle is quite simple and straightforward.
First, the spinal needle is introduced into the guide needle as far as
the distal end of the latter. Then, the now Eldor needle is introduced
into the selected intervertebral space and the epidural space is located
using the well-known indicator methods. After that the epidural catheter
is introduced into the epidural space, confirming its position by the test
dose technique. Then, the spinal needle is slowly pushed in to puncture
the dura, until cerebrospinal fluid is obtained. The anesthetic solution
is injected through the spinal needle into the spinal space. Subsequently,
the spinal needle is slowly withdrawn from the guide needle and then the
Eldor needle is withdrawn, leaving the epidural catheter in position in
the epidural space. 1. Eldor J, Guedj P. Une nouvelle auguille pour l`anesthesie
rachidienne et peridurale conjointe. Ann Fr Anesth Reanim 1990;9:571-572
Huber needle technique
Huber (1), the inventor of the "Tuohy" epidural needle, also patented
in 1953 an hypodermic needle with an "auxiliary outlet being disposed in
transverse alignment with the channel outlet" (2). Hanaoka (3) described
in 1986 its use in 500 patients. This needle has a very small hole behind
the epidural needle tip ("back eye"). A small gauge spinal needle is inserted
through that hole and punctures the dura. After withdrawing the spinal
needle an epidural catheter is introduced through the epidural needle.
1. Eldor J. Huber needle and Tuohy catheter. Reg Anesth 1995;20:252-253
2. Huber RL. Hypodermic needle. US Patent No. 2,748,769 3. Hanaoka K. Experience
in the use of Hanaoka`s needles for spinal-continuous epidural anaesthesia
(500 cases). 7th Asian Australasian Congress of Anaesthesiologists Abstracts.
Hong Kong, 1986;161-162
Eldor, Coombs and Torrieri technique
Eldor (1) and Torrieri (2) described in separate letters, in 1988, an
epidural needle with a spinal needle attached to it. Through the spinal
needle a longer spinal needle is inserted into the subarachnoid space,
while an epidural catheter is introduced through the epidural needle into
the epidural space. A few months before the publication of these letters,
Coombs (3) applied for a patent on the same device. 1. Eldor J, Chaimsky
G. Combined spinal-epidural needle (CSEN). Can Anaesth Soc J 1988;35:537-8
2. Torrieri A, Aldrete JA. Letter to the Editor. Acta Anaesthesiologica
Belgica 1988;39:65-66 3. Coombs DW. Multi-lumen epidural-spinal needle.
US Patent No. 4,808,157
Indications
Combined spinal-epidural anesthesia is like "to paint the fence" from
both its sides. The indications are those of the spinal or epidural alone
and even more. Rawal (1) made a survey in 17 European countries on their
anesthetic choices in 1992. 17% of the procedures were performed under
central blocks. Among these blocks - 56% were spinal; 40% - epidural and
4% - combined spinal-epidural anesthesia. The commonest indication for
combined spinal-epidural blocks was hip replacement surgery (28.2%), followed
by hysterectomy (19%), knee surgery (14.4%), Cesarean section (14%), emergency
Cesarean section (13%), femur fracture in elderly patients (7.2%) and prostatectomy
(5.6%). This under-utility of regional anesthesia (only 17% of the procedures)
is in contrast to how the anesthesiologists would like to be anesthetized
in case they need an operation: In 1986, Broadman et al. (2) confirmed
that 92% of the anesthesiologists preferred regional over general anesthesia
for their own hypothetical surgery, while 74% preferred a regional technique
for their own elective extremity surgery. This is in accordance with a
previous survey done in 1973 by Katz (3) in which 68% of the American anesthesiologists
surveyed preferred regional anesthesia for their own anesthetic during
an unspecified elective surgical procedure. The spectrum of indications
for the combined spinal-epidural anesthesia ranges from labor analgesia
(4,5) to high abdominal and even thoracic and head operations (6) by the
adjuvant use of an endotracheal tube ventilation. The dosages of the local
anesthetics with or without opioids that are injected into the spinal and
epidural spaces are now evaluated in various hospitals around the world.
The dosage combinations are enormous. The story has only begun. 1. Rawal
N. European trends in the use of combined spinal epidural technique - A
17-nation survey. Reg Anesth 1995;20 (Suppl):162 2. Broadman LM, Mesrobian
R, Ruttiman U, McGill WA. Do anesthesiologists prefer a regional or a general
anesthesia for themselves? Reg Anesth 1986;11:557 3. Katz J. A survey of
anesthetic choice among anesthesiologists. Anesth Analg 1973;52:373-5 4.
Abouleish A, Abouleish E, Camann W. Combined spinal-epidural analgesia
in advanced labour. Can J Anaesth 1994;41:575-8 5. Arkoosh VA, Sharkey
SJ, Norris MC, Isaacson W, Honet JE, Leighton BL. Subarachnoid block analgesia:
Fentanyl and morphine versus fentanyl and morphine. Reg Anesth 1994;19:243-246
6. Eldor J. Combined spinal-epidural-general anesthesia. Reg Anesth 1994;19:365-6
Problems
Blumgart et al. (1) found that the mechanism of extension of spinal
anesthesia by extradural injection of local anesthetics is largely a volume
effect. Using extradural saline 10 ml and extradural bupivacaine 0.5% 10
ml - the extension of the block was found to be similar in the saline or
the bupivacaine groups, and significantly faster than the group which received
no extradural injection after spinal injection of 1.6-1.8 ml of 0.5% hyperbaric
bupivacaine. Suzuki et al. (2) found that spinal puncture with a 26 gauge
spinal needle, with no spinal anesthetic injection, immediately before
epidural injection of 18 ml 2% mepivacaine resulted in rapid caudal spread
of analgesia as compared to an epidural anesthetic alone. They attributed
it to the flow of local anesthetic into the subarachnoid space through
the perforation produced by the spinal needle. In all the techniques, except
the Eldor needle and Curelaru`s double-space techniques, there is inability
to perform the epidural catheter test dose due to the fact that the epidural
catheter is inserted after the subarachnoid local anesthetic injection.
This can result in epidural catheter malposition in the subarachnoid space
or intravascular with a danger of total spinal, delayed cardiorespiratory
arrest due to opioid overdosage (3,4) or convulsions. Due to the insertion
of the spinal needle through the bent tip of the epidural needle in the
needle-through-needle technique there is friction that produces metallic
microparticles that can be introduced further into the epidural space by
the epidural catheter insertion (5,6). If there is a delay in epidural
catheter threading in the needle-through-needle technique there is a partial
spinal anesthesia while using the hyperbaric anesthetic solution (7), with
the need to supplement it further through the epidural route. The incidence
of epidural needle or catheter unintentional dural puncture ranges from
2.5% (8) to 0.6% (9) and even 0.26% (10). However, using the needle-through-needle
technique the chances are greater because of the same pathway shared by
the spinal needle and the epidural catheter in the epidural space and the
force exerted by the friction between the spinal needle and the epidural
needle`s tip that can advance forward the epidural needle causing an unrecognized
dural tear by the epidural needle, through which an epidural catheter can
be threaded inadvertently. 1. Blumgart CH, Ryall D, Dennison B, Thompson-Hill
LM. Mechanism of extension of spinal anaesthesia by extradural injection
of local anaesthetic. Br J Anaesth 1992;69:457-460 2. Suzuki N, Koyanemaru
M, Onizuka S, Takasaki M. Dural puncture with a 26-gauge spinal needle
affects epidural anesthesia. Reg Anesth 1995;20 (Suppl):118 3. Myint Y,
Bailey PW, Milne BR. Cardiorespiratory arrest following combined spinal
epidural anaesthesia for caesarean section. Anaesthesia 1993;48:684-686
4. Eldor J, Guedj P, Levine S. Delayed respiratory arrest in combined spinal-epidural
anesthesia. Reg Anesth 1994;19:418-422 5. Eldor J, Brodsky V. Danger of
metallic particles in the spinal-epidural spaces using the needle-through-needle
approach. Acta Anaesthesiol Scand 1991;35:461 6. Eldor J. Metallic particles
in the spinal-epidural needle technique. Reg anesth 1994;19:219-220 7.
Fan SZ, Susetio L, Wang YP, Cheng YJ, Liu CC. Low dose of intrathecal hyperbaric
bupivacaine combined with epidural lidocaine for cesarean section - a balance
block technique. Anesth Analg 1994;78:474-7 8. Dawkins CJM. An analysis
of the complications of extradural and caudal block. Anaesthesia 1969;24:554-563
9. Tanaka K, Watanabe R, Harada T, Dan K. Extensive application of epidural
anesthesia and analgesia in a university hospital: Incidence of complications
related to technique. Reg Anesth 1993;18:34-38 10. Macdonald R, Lyons G.
Unintentional dural puncture, Anaesthesia 1988;43:705
The twin theory
Spinal anesthesia is a safe, cost-effective and reliable form of anesthesia.
Many anesthesiologists would regard the epidural as an insurance against
unsatisfactory spinal anesthesia, aiming to provide complete anesthesia
by the subarachnoid route (1). Another approach is the use of a minimal
dose of spinal anesthesia for a shorter duration with the flexibility of
epidural reinforcement if necessary. For many years in many anesthetic
departments around the world there was a philosophy that extradurals are
for young people and the intrathecal route for the old, with few exceptions.
Seeberger et al. (2) addressed the question: Is the spinal or the epidural
technique better? Two hundred and two patients younger than 50 years underwent
spinal or epidural anesthesia. Spinals were performed with 24-gauge Sprotte
needles and epidurals with 18 gauge Tuohy needles and catheters. The failure
rate of both techniques was 5%. Patient acceptance was high in both groups
(97% in the spinal; 93% in the epidural). The authors concluded that spinal
anesthesia was superior, because of better quality of anesthesia, no risk
of intoxication, less time needed to perform the block, and less expensive
kits. However, using the combined spinal-epidural anesthesia there is no
more a question of which is better, as Greene and Brull (3) wrote: "Epidural
and spinal anesthesia are indeed related to each other, but only to the
same extent as cousins, or, at best, siblings; monozygotic twins they are
not". 1. Brownridge P. Epidural and subarachnoid analgesia for elective
caesarean section. Anaesthesia 1981;36:70 2. Seeberger MO, Lang ML, Drewe
J, Schneider M, Hauser E, Hruby J. Comparison of spinal and epidural anesthesia
for patients younger than 50 years of age. Anesth Analg 1994;78:667-73
3. Greene NM, Brull SJ. Physiology of spinal anesthesia. 4th ed. Baltimore:Williams
& Wilkins, 1993, p.IX
Failed Spinal or Epidural Anesthesia
Failure of regional anesthesia has been reported to be in the order
of 4% (1,2). The failure rate of spinal anesthesia alone ranged between
3.1% - 17% involving 100 to 1,891 patients respectively (3,4). Johr et
al. (5) investigated the incidence of failed spinal anesthesia in a Swiss
teaching institution. Of 3,004 blocks 197 (6.5%) did not provide satisfactory
analgesia. The 197 failures included: absent blockade - 36; failure to
obtain CSF - 6; level too low - 90; duration too short - 36; intensity
too weak - 28; unclear - 1. However, 531 (17.4%) blocks were excessively
high (45 - cervical level; 2 - required intubation). The management of
the 197 failed blocks included: additional spinal anesthesia - 117; epidural
anesthesia - 2; local infiltration - 1; general anesthesia - 30; IV supplementation
- 47. Manchikanti et al. (6) found that the failure rate with sole use
of spinal anesthesia ranges between 0.46% and 35% . Epidural analgesia
sometimes falls short of perfection due to the variable "compartmentalisation"
of the epidural space (7). Shesky et al. (8) studied in 1983 the dose-response
of bupivacaine for spinal anesthesia. Sixty males having transurethral
surgery were studied using 10-, 15- and 20 mg doses of glucose-free bupivacaine
as either a 0.5 or a 0.75% solution. Both 15 and 20 mg of either concentration
of bupivacaine provided satisfactory spinal anesthesia. However, three
of 20 patients receiving 10 mg dose required supplementation with general
anesthesia. Lyons et al. (9) used a 26G spinal needle through the Tuohy
epidural needle for the combined spinal-epidural anesthesia. Unsuccessful
spinal anesthesia occurred in 8 of the 50 patients (16%). In four patients,
anesthesia was provided by the epidural route, while in the remainder another
intrathecal injection was made using a different intervertebral space.
Lesser et al. (10) evaluated the use of a 30G spinal needle through the
Tuohy epidural needle for the combined spinal-epidural anesthesia. Unsuccessful
spinal anesthesia was in 12 of the 50 patients (24%) studied. Six failures
were due to unsuccessful dural puncture and six to inadequate block. Due
to requirement of large doses of local anesthetics for epidural block there
is a risk of toxic complications (11,12). In spite of large doses epidural
block may fail to provide adequate analgesia in up to 25% of patients due
to difficulty in blocking sacral roots (13-15). Failure to obtain CSF when
using the needle-through-needle technique may occur despite successful
dural puncture if the needle orifice is occluded, for example by a nerve
root. It may also happen if dural puncture has failed to occur because
the spinal needle is too short or is placed too laterally as the epidural
needle may have entered the epidural space at an angle (16). One technical
problem of the needle-through-needle method is the occasional difficulty
in threading the catheter into the epidural space after injection of the
spinal solution. If some minutes are spent in replacing the epidural needle,
the spinal solution may become relatively "fixed" on the dependent side
(17). However, when spinal and epidural anesthesia are combined, recourse
to general anesthesia becomes a very rare event. 1. Milne MK, Lawson JIM.
Epidural analgesia for Caesarean section. A review of 182 cases. Br J Anaesth
1973;45:1206-10 2.Moir DD. Local anaesthetic techniques in obstetrics.
Br J Anaesth 1986;58:747-59. 3. Tarkkila PJ. Incidence and causes of failed
spinal anesthetics in a university hospital: a prospective study. Reg Anesth
1991;16:48-51 4. Levy JH, Islas JA, Ghia JN, Turnbull C. A retrospective
study of the incidence and causes of failed spinal anesthetics in a university
hospital. Anesth Analg 1985;64:705-10 5. Johr M, Hess FA, Balogh S, Gerber
H. Incidence and management of failed spinal anaesthesia in a teaching
institution: A prospective evaluation of 3,004 epidural blocks. Acta Anaesthesiol
Scand 1995;39:A421 6. Manchikanti L, Hadley C, Markwell SJ, Colliver JA.
A retrospective analysis of failed spinal anesthetic attempts in a community
hospital. Anesth Analg 1987;66:363-6. 7. Husemeyer RP, White DC. Topography
of the lumbar epidural space. A study in cadavers using injected polyester
resin. Anaesthesia 1980;35:7-11. 8. Sheskey MC, Rocco AG, Bizzari-Schmid
M, Francis DM, Edstrom H, Covino BG. A dose-response study of bupivacaine
for spinal anesthesia. Anesth Analg 1983;62:931-5. 9. Lyons G, Macdonald
R, Mikl B. Combined epidural/spinal anaesthesia for Caesarean section:
Through the needle or in separate spaces? Anaesthesia 1992;47:199-201.
10. Lesser P, Bembridge M, Lyons G, Macdonald R. An evaluation of a 30-gauge
needle for spinal anaesthesia for Caesarean section. Anaesthesia 1990;45:767-8.
11. Abouleish E, Bourke D. Concerning the use and abuse of test doses for
epidural anesthesia. Anesthesiology 1984;61:344-5. 12. Thorburn J, Moir
DD. Bupivacaine toxicity in association with extradural analgesia for Caesarean
section. Br J Anaesth 1984;56:551-3. 13. Larsen JV. Obstetric analgesia
and anaesthesia. Clinics in Obst Gyn 1982;9:685-710. 14. Thorburn J, Moir
DD. Epidural analgesia for elective Caesarean section. Technique and its
assessment. Anaesthesia 1980;35:3-6. 15. Kileff ME, James FM, Dewan DM,
Floyd HM. Neonatal neurobehavioral responses after epidural anesthesia
for Cesarean section using lidocaine and bupivacaine. Anesth Analg 1984;63:413-7.
16. Patel M, Samsoon G, Swami A, Morgan BM. Flow characteristics of long
spinal needles. Anaesthesia 1994;49:223-225. 17. Carrie LES. Epidural versus
combined spinal epidural block for Caesarean section. Acta Anaesthesiol
Scand 1988;32:595-596.
One needle technique for combined spinal-epidural anesthesia
Vitenbeck (1), in 1980, described the use of combined spinal-epidural
anesthesia in 210 patients using the same needle for the spinal and the
epidural injections. He first injected 1-2 ml Dicaine 0.2% into the subarachnoid
space. Five minutes later he injected through the same needle, which was
withdrawn into the epidural space, 25-37 ml of Dicaine 0.2-0.3% in distilled
water with adrenaline 1:1,000. Anesthesia lasted for 2.5-3.5 hr. In only
3 patients he needed to induce general anesthesia because the operation
lasted more than the effect of the regional anesthesia. Only 2 patients
(0.9%) had postdural puncture headaches. 1. Vitenbeck IA. Associated spino-peridural
anesthesia as a variant of conduction anesthesia during operation. Vestn
Khir 1981;126:123-128.
Aspiration pneumonia prevention by the CSEA
In a review of maternal mortality published in 1991 (1) Glassenberg
quoted statistics collected up to the mid-1980`s in the UK, USA and Sweden.
Over the preceding decade, aspiration as a cause of maternal death had
fallen to two deaths per million births, or one death per 30,000 anesthetics,
still seven times the aspiration fatality rate for the non-obstetric surgical
population, and closely associated with failed intubation. Dennis W. Coombs
(2) wrote in 1983 an editorial entitled "Aspiration pneumonia prophylaxis".
He said that "unfortunately, the magic prophylactic bullet is not available
yet for all situations". However, instead of a "cimetidine prophylaxis"
it is suggested to use the "CSEA prophylaxis"... 1. Glassenberg R. General
anaesthesia and maternal mortality. Semin Perinatol 1991;15:386-396. 2.
Coombs DW. Aspiration pneumonia prophylaxis. Anesth Analg 1983;62:1055-8.
Intraoperative challenges
Although developments in anesthesia and surgery have improved overall
surgical outcome during recent decades, there is still concern about the
detrimental effects of operative procedures, such as myocardial infarction,
pulmonary complications, thromboembolism, gastrointestinal paralysis, immunosuppression,etc.,
that cannot be attributed solely to imperfections in surgical technique
(1). Edwards et al. (2) studied 100 patients undergoing transurethral surgery,
who were allocated randomly to receive either general or spinal anesthesia.
The overall incidence of myocardial ischemia increased from 18% to 26%
between the preoperative and postoperative periods, but no significant
difference between the two anesthetic techniques. Nakatsuka et al. (3)
used spinal anesthesia combined with epidural anesthesia in nine patients
with ischemic heart disease having femoral-distal artery bypass surgery.
A 20-gauge epidural catheter and a 24-gauge spinal catheter were inserted.
Epidural anesthesia was initiated using 10-12 ml of 2% lidocaine and switched
to continuous epidural anesthesia with 0.5% bupivacaine (5-7 ml/hr). Spinal
bupivacaine 0.75% was injected up to 5 mg through the spinal catheter as
needed to manage surgical pain of lower leg and foot. Seven out of 9 patients
required additional spinal anesthesia. Juelsgaard et al. (4) examined continuous
spinal anesthesia vs single dose spinal anesthesia vs general anesthesia
in 44 elderly patients scheduled for hip surgery and receiving medication
for angina or displaying ECG signs of coronary sclerosis. In the continuous
spinal anesthesia they injected 1.5 ml isobaric bupivacaine 0.5% with 0.5
ml increments to establish T10 anesthesia. In the single dose spinal anesthesia
group they injected 2.5 ml isobaric bupivacaine 0.5%. The general anesthesia
consisted of fentanyl, thiopentone, N2O/O2 and enflurane. There were only
3 hypotensive events in the continuous spinal group (3/10 patients) compared
to 24/13 patients in the single dose spinal group and 29/11 patients in
the general anesthesia group. There was only 1 ischemic event in the continuous
spinal group compared to 93 ischemic events in the single dose spinal and
11 in the general anesthesia group. These benefits of continuous spinal
anesthesia can be obtained also in the combined spinal-epidural anesthesia,
while the spinal injections can be done in incremental doses of 0.5 ml
plain bupivacaine through the spinal needle or at a reduced dose of 1-1.5
ml injected slowly into the spinal space, and then supplemented by the
epidural route, if necessary. 1. Kehlet H. Postoperative pain relief: A
look from the other side. Reg Anesth 1994;19:369-377. 2. Edwards ND, Callaghan
LC, White T, Reilly CS. Perioperative myocardial ischemia in patients undergoing
transurethral surgery: a pilot study comparing general with spinal anaesthesia.
Br J Anaesth 1995;74:368-372. 3. Nakatsuka M, Long SP, Shy DG. Spinal anesthesia
combined with epidural anesthesia for peripheral vascular emergency with
dual catheters. Anesth Analg 1994;78:S309. 4. Juelsgaard P, Sand NPR, Felsby
S, Dalsgaard J, Brink O, Thygesen K. Continuous spinal anaesthesia vs single
dose spinal anaesthesia vs general anaesthesia: Perioperative holter monitoring
of patients with coronary atherosclerosis. Acta Anaesthesiol Scand 1995;39:A428
Anesthesia and public image
Swinhoe and Groves (1) pinponted again the low public image of anaesthesiology
and anaesthesiologists. Their paper was commented by anaesthesiologists
from other countries who showed the same trend (2,3). Keep and Jenkins
(4) showed in 1978 the same finding that only 67% (65% in Swinhoe and Groves`
report) of the patients thought an anaesthesiologist was a medical doctor.
Their conclusion was that there is a need to give information sheets to
patients preoperatively on the ward. It is possible to attack this genuine
problem from another point of view: In 1973, Katz (5) surveyed American
anesthesiologists and found that 68% preferred regional anaesthesia for
their own anaesthetic during an unspecified elective surgical procedure.
In 1986, Broadman et al (6) confirmed that a majority of anaesthesiologists
still preferred regional over general anaesthesia for their own extremity
surgery. In their survey, 92% of the anaesthesiologists preferred regional
over general anaesthesia for their own hypothetical emergency surgery,
while 74% preferred a regional technique for their own elective extremity
surgery. It is possible that if most anaesthetics are done by the regional
techniques there will be much time for the awakened patient to learn that
the person at the top of the operating table is not less important than
the person who stands behind the sterile curtain... and both of them are
medical doctors. So, anesthesiologists have to treat their patients as
they would like to be treated while they are patients - and they have already
chosen : Regional anaesthesia. This shift in the anaesthetic profession
towards the regional techniques will be also a shift in the public recognition
and appreciation of anesthesiology and anesthesiologists. 1. Swinhoe CF,
Groves ER. Patient`s knowledge of anaesthetic practice and the role of
anaesthetists. Anaesthesia 1994;49:165-6. 2. Gajraj NM, Bala AS. Patient`s
knowledge of anaesthetists. Anaesthesia 1994;49:559. 3. Ali S, Vivekanaandan
P, Tierney E. Patient`s perception of the anaesthetist and anaesthesia.
Anaesthesia 1994;49:644-5. 4. Keep PJ, Jenkins JR. As others see us. The
patient`s view of the anaesthetist. Anaesthesia 1978;33:43-5. 5. Katz J.
A survey of anesthetic choice among anesthesiologists. Anesth Analg 1973;52:373-5.
6. Broadman LM, Mesrobian R, Ruttiman U, McGill WA. Do anesthesiologists
prefer a regional or a general anesthetic for themselves? Regional Anesthesia
1986;11:S57.
Huber needle and Tuohy catheter
On April 23, 1941, Edward B. Tuohy (1) presented his experience of continuous
spinal anesthesia in the Proceedings of the Staff Meetings of the Mayo
Clinic. The method of continuous spinal anesthesia was first used in the
Mayo Clinic in November 1940 according to the technic and equipment advocated
by William T. Lemmon (2). It consisted of a special operating table mattress,
special spinal needles, 18 gauge, with stylet, which were soft and malleable,
a 10 ml Luer-lok syringe with special stopcock connections and rubber tubing
to connect the spinal needle with the glass syringe. The rubber-covered
mattress had a gap 7 inches (18 cm) in length which lied beneath the lumbar
portion of the spinal column when the patient was lying on the mattress.
Three years later, on March 1944, Tuohy (3) described an alternative method
in lieu of a malleable needle for continuous spinal anesthesia: Use of
an ureteral catheter. The idea of using an ureteral catheter for continuous
spinal anesthesia came to Captain Tuohy, who served then in the Medical
Corps, Army of the United States, from the reports of the use of the ureteral
catheter for caudal anesthesia (4,5) and for continuous subarachnoid drainage
of meningitis advocated by Love (6). On June 14, 1944, Major Tuohy (7)
who was then the chief of anesthesia and operative section, Percy Jones
General Hospital, Battle Creek, Mich., described this technic before the
section on Anesthesiology at the Ninety-Fourth Annual Session of the American
Medical Association in Chicago. In the following article published on May
26, 1945 in JAMA Tuohy (7) said that "the direction (cephalad or caudad)
which the catheter will advance in the subarachnoid space after the tip
of the catheter leaves the end of the guiding needle cannot be predicted
positively; however, if the round tip of the catheter is bent slightly
before it is introduced into the lumen of the needle, I have found that
the catheter will advance cephalad in most cases". In a later article published
in 1945 Tuohy (8) mentioned for the first time a 15 gauge needle with Huber
point. Using this kind of needle he could "direct the catheter either cephalad
or caudad as desired". No reference was given by Tuohy to the use of the
name of Huber. Cousins and Bridenbaugh (9) in their textbook on Neural
Blockade mentioned that Tuohy "performed continuous spinal anesthesia by
means of a ureteral catheter introduced in the subarachnoid space through
a needle with a Huber point". No reference is given to the "Huber point",
besides that of Tuohy, who also did not give any reference, as noticed
before. Ronald Miller (10) in his textbook of Anesthesia gives a nice photograph
of an "18-gauge Huber needle for continuous spinal catheter insertion",
but with no reference. No other textbook in anesthesia tells us who was
Huber whom his needle or his "point" revolutionized regional anesthesia.
Medline search gave only articles on Huber-point needle in the port-a-cath
implantable device, but with no reference to the question of who was Huber
or when did he first describe his needle or his "point". The point is that,
there is no reference in the medical literature of Huber`s description
of his needle. A search in U.S. patents brought to U.S. patent No. 2,409,979
applied on March 14, 1946 by Ralph L. Huber from Seattle, Washington. He
described there an hypodermic needle with a "transversely curved wall...end
portion". In a recent correspondence said Winnie AP (11) that "history
will recall what is published, not what is patented; and no subsequent
publication will make up for failure to describe a new piece of technology
in the medical literature". Winnie is right, at least for the last 50 years
concerning Huber`s contribution to anesthesia. However, there is some injustice
in the history of anesthesia on that subject. Every anesthesiologist knows
what is the Tuohy needle. No anesthesiologist till now knows that the Tuohy
needle is the Huber needle. Tuohy only used it for the introduction of
the Tuohy catheter. I do not believe that all the companies which sell
these "Tuohy needles" will change now its name to Huber needles, but maybe
in the year 2,045... 1. Tuohy EB. Continuous spinal anesthesia. Proceedings
of the Staff Meetings of the Mayo Clinic 1941;17:257-259. 2. Lemmon WT.
A method for continuous spinal anesthesia. Ann Surg 1940;111:141-144. 3.
Tuohy EB. Continuous spinal anesthesia: its usefulness and technic involved.
Anesthesiology 1944;5:142-148. 4. Adams RC, Lundy JS, Seldon TH. Continuous
caudal anesthesia or analgesia: a consideration of the technic , various
uses and some possible dangers. JAMA 1943;122:152-158. 5. Manalan SA. Caudal
block anesthesia in obstetrics. J Indiana M. A. 1942;35:564-565. 6. Love
JG. Continuous subarachnoid drainage of meningitis by means of a ureteral
catheter. JAMA 1935;104:1595. 7. Tuohy EB. The use of continuous spinal
anesthesia utilizing the ureteral catheter technic. JAMA 1945;128:262-264.
8. Tuohy EB. Continuous spinal anesthesia: A new method utilizing a ureteral
catheter. Surg Clins N. Am 1945;25:834-840. 9. Cousins MJ, Bridenbaugh
PO. Neural Blockade in Clinical Anesthesia and Management of Pain. J.B.
Lippincott Co., 2nd ed. 1988;p.11. 10. Miller RD. Anesthesia. 3rd ed.,
Churchill Livingstone 1990;Fig. 45-8. 11. Winnie AP. A letter to Ostheimer
GW. March 17, 1994.
Total spinal anesthesia: The origin of CSEGA
Evans (1) described in 1928 the possible complications of spinal anesthesia.
Concerning respiratory paralysis he wrote:" If respiration should cease
, keep cool. Raise the lower jaw, pull the tongue forward and begin artificial
respiration at a uniform rate. Mouth to mouth insufflation is the most
convenient and efficacious method of artificial respiration". Twenty years
before, in September 1908, before the Congress of the International Society
of Surgery, in Brussels, Thomas Jonnesco (2) from Bucharest, described
his new method of general spinal anesthesia and reported 14 cases operated
upon by his method. Bier, who 10 years ago established the first human
surgical spinal anesthesia, rejected it (2). In a later paper in 1910 Jonnesco
wrote: "It is an error to confuse lumbar rachianesthesia, conceived by
Corning and popularized by Bier, with my method. As I have many times emphasized
, my method is a new one and altogether distinctive, because I have generalized
spinal anaesthesia , adopting it to all operations on any part of the body"
(3). Patients given high spinal anesthesia frequently either lapse into
what appears to be normal sleep or may actually lose consciousness (4-7).
If patients with high spinal anesthesia are given an inhalational anesthetic
such as nitrous oxide-oxygen , very low concentrations of anesthetic gases
are required to maintain unconsciousness (8). Reduction in the strength
of nociceptive input may contribute to loss of consciousness by diminishing
the strength of arousing stimuli arriving at cortical structures (9). Studies
with C14 labeled lidocaine in dogs have shown that the foramen magnum is
not a physiological barrier, for autoradiographs and tissue samples reveal
the presence of radioactivity in intracranial parts of the CNS after a
relatively modest epidural dose (10). Total spinal anesthesia has been
used as a method of general anesthesia for abdominal surgery (11) and for
the treatment of intractable pain (12). Gillies and Morgan (13) described
a patient in whom a total spinal anesthesia resulted after 18 ml of inadvertent
subarachnoid injection of 0.5% bupivacaine. Spontaneous respiration was
noted 120 minutes later and consciousness regained after further 65 minutes.
Return of respiration after 17 ml 1.5% lignocaine which resulted in total
spinal analgesia occurred after 45 minutes and consciousness after further
80 minutes (14). Four patients with intractable pain were treated by total
spinal anesthesia. Power spectral analysis of heart rate and peripheral
blood flow variations were studied. Vagal activity was depressed as well
as the sympathetic activity innervating the cardivascular system, so the
heart rate and peripheral blood flow variations were totally eliminated
(15). Total spinal block can be elicited even after an epidural test dose
like the 36 year old parturient of Palkar et al. (16) who developed hypotension
and extensive sensory and motor block including respiratory paralysis and
aphonia after injection via the epidural catheter of 3 ml lidocaine 1.5%
(45 mg) with 1:200,000 epinephrine (15 microgram). The patient remained
fully conscious and alert and spontaneous respiration recommenced in five
minutes. Three patients were studied to determine the changes in regional
skin temperature and blood flow during extensive sympathetic blockade following
total spinal anesthesia. The temperature of the truncal area, arm and leg
decreased by 1 degree C, whereas the temperature of the hand and foot increased
by 3 degrees C (17). Total spinal block was induced by 2% lidocaine in
adult mongrel dogs. Heart rate, mean arterial pressure, cardiac index and
left ventricle dp/dt max decreased significantly (18). Ephedrine 0.5 mg/Kg
elevated HR, MAP, LV dp/dt max and SVR (19). Total spinal anesthesia blocks
the vagus as well as the sympathetic nervous system and decreases heart
rate variation, suggesting that neural control of the heart via the autonomic
nervous system is abolished after total spinal anesthesia (17). Matsuki
et al. (20) described a patient with primary aldosteronism who was anesthetized
by total spinal anesthesia using an epidural catheter inserted at L3-4
into the subarachnoid space. The trachea was intubated after intravenous
injection of thiopentone 250 mg and suxamethonium 40 mg, and oxygen 3 liters/minute
and nitrous oxide 2 liters/minute inhaled. The intraoperative course was
smooth and intraoperative muscle relaxation excellent. Adrenaline, noradrenaline
and dopamine in the plasma remained within normal ranges. Mets et al (21)
described a case of an unplanned version of CSEGA: A 24 year old parturient
received an epidural analgesia during labor. Then she was scheduled for
cesarean section for failure to progress. A total dose of 30 ml 0.5% bupivacaine
was administered incrementally via the epidural catheter which resulted
in a patchy block that was inadequate for surgery. Twenty minutes after
the last injection of epidural local anesthetic a spinal anesthesia was
done which resulted in a high block that necessitated tracheal intubation
and ventilation. Controlled ventilation maintained with 50% N2O and 0.5%
isoflurane in oxygen until delivery of the baby after which the isoflurane
was stopped and 70% N2O in oxygen was administered. No further muscle relaxation
was required for the remainder of the operation which lasted 45 minutes.
The patient was extubated at the end of the operation uneventfully. 1.
Evans CH. Possible complications with spinal anesthesia. Their recognition
and the measures employed to prevent and to control them. Am J Surgery
1928;5:581-593. 2. Jonnesco T. Remarks on general spinal analgesia. Br
Med J 1909;2:1396-1401. 3. Jonnesco T. Concerning general rachianesthesia.
Am J Surgery 1910;24:33 4. Koster H, Kasman LP. Spinal anesthesia for the
head, neck and thorax: its relation to respiratory paralysis. Surg Gynecol
Obstet 1929;49:617. 5. Vehrs GR. Spinal anesthesia: Technic and clinical
application. St Louis : The C.V. Mosby Co., 1934. 6. Jones RGG. A complication
of epidural technique. Anaesthesia 1953;8:242. 7. Huvos MC, Greene NM,
Glaser GH. Electroencephalographic studies during acute subtotal denervation
in man. Yale J Biol Med 1962;34:592. 8. Greene NM. Hypotensive spinal anesthesia.
Surg Gynecol Obstet 1952;95:331. 9. Kendig JJ. Spinal cord as a site of
anesthetic action. Anesthesiology 1993;79:1161-2. 10. Bromage PR, Joyal
AC, Binney JC. Local anaesthetic drugs: Penetration from the spinal extradural
space into the neuraxis. Science 1963;140:392. 11. Evans TI. Total spinal
anaesthesia. Anaesth Intensive Care 1974;2:158-63. 12. Yamashiro H, Hirano
K. Treatment with total spinal block of severe herpetic neuralgia accompanying
median and ulnar nerve palsy. Masui 1987;36:971-5. 13. Gillies IDS, Morgan
M. Accidental total spinal analgesia with bupivacaine. Anaesthesia 1973;28:441-5.
14. DeSaram M. Accidental total spinal analgesia. A report of three cases.
Anaesthesia 1956;11:77. 15. Goda Y, Kimura T, Goto Y, Kemmotsu O. Power
spectral analysis of heart rate and peripheral blood flow variations during
total spinal anesthesia. Masui 1989;38:1275-81. 16. Palkar NV, Boudreaux
RC, Mankad AV. Accidental total spinal block : a complication of an epidural
test dose. Can J Anaesth 1992;39:1058-60. 17. Kimura T, Goda Y, Kemmotsu
O, Shimada Y. Regional differences in skin blood flow and temperature during
total spinal anaesthesia. Can J Anaesth 1992;39:123-7. 18. Kobori M, Negishi
H, Masuda Y, Hosoyamada A. Changes in respiratory , circulatory, endocrine,
and metabolic systems under induced total spinal block. Masui 1991;40:1804-9.
19. Kobori M, Negishi H, Masuda Y, Hosoyamada A. Changes in systemic circulation
under induced total spinal block and choice of vasopressors. Masui 1990;39:1580-5.
20. Matsuki M, Muraoka M, Oyama T. Total spinal anaesthesia for a Jehovah`s
Witness with primary aldosteronism. Anaesthesia 1988;43:164-5. 21. Mets
B, Broccoli E, Brown AR. Is spinal anesthesia after failed epidural anesthesia
contraindicated for cesarean section? Anesth Analg 1993;77:629-31.
What is anesthesia?
Definitions of the state of anesthesia: 1. Drug-induced unconsciousness;
the patient neither perceives nor recalls noxious stimulation (1). 2. Reversible
oblivion and immobility (2). 3. Paralysis, unconsciousness, and attenuation
of the stress response (3). 4. Sensory block, motor block, blocking of
reflexes, and mental block (4). 5. All separate effects used to protect
the patient from the trauma of surgery (5). Jorgensen et al. (6) studied
the anesthetic choice of 705 patients of outpatient surgery candidates
prior to speaking to the anesthesiologist. Sixty five percent preffered
general anesthesia, 22% - spinal anesthesia, and 12% were unsure. Of those
who had spinal anesthesia previously, only 33% would select it in the future.
Conversely, 70% of patients who had general anesthesia would prefer it
again. Concerns about spinal anesthesia were : paralysis, nerve damage,
being awake, infection, inadequate anesthesia, backache, fear of needle
and headache. The use of regional anesthesia in residency training programs
has increased from 21.3% in 1980 to 29.8% in 1990, primarily because of
a two-fold rise in the use of epidural anesthesia (7). Advantages of spinal
anesthesia: Obviates the need for deep general anesthesia, profound muscle
relaxation, cheap, easy to perform, danger of toxic drug signs - negligible.
Disadvantages of spinal anesthesia: hypotension, postoperative headache,
some patients prefer to be asleep during operation. The combined spinal-epidural
anesthesia combines the rapid onset and good muscle relaxation of subarachnoid
block with the ability to supplement analgesia through the epidural catheter,
intraoperatively and after the operation. Reynolds et al. (8) using plain
lumbar x-rays and CT after injection of iodized oil into the extradural
space of 19 subjects recorded the depth of the extradural space at the
caudal end: 8.3 ±1.95 mm (at the level of T12). Westbrook et al.
(9) found even a smaller ligamentum flavum-dura mater depth at the L2-3
level: 3.95±1.1 mm by using the magnetic resonance imager of 39
subjects. Pitkin (10) describing spinal anesthesia in 1928 wrote that "in
1912, its use was confined to very elderly people, those considered as
`bad risks` and to whom we were afraid to give ether". Koster (11) described
in 1928 his experience of spinal anesthesia also in operations of the head,
neck and thorax. He wrote: "Any one who can do a lumbar puncture can induce
spinal anesthesia; the method is reasonably `fool proof` ". Babcock (12)
in 1928 summarized his experience of 24 years with spinal anesthesia: "In
no other known way can so profound and extensive an anesthesia be produced
by so small a dose of a drug and with so little general toxicity". Bromage
(13) stated in 1967 that "the beautiful precision and economy of a subarachnoid
block is lacking in epidural anesthesia". Greene and Brull (14) in their
preface to the fourth edition of "Physiology of Spinal Anesthesia" have
written: "Epidural and spinal anesthesia are indeed related to each other,
but only to the same extent as cousins or, at best, siblings; monozygotic
twins they are not". 1. Prys-Roberts C. Anaesthesia: a practical or impractical
construct? Br J Anaesth 1987;59:1341-5. 2. Eger EI. What is general anesthetic
action? Anesth Analg 1993;77:408-9. 3. Pinsker MC. Anesthesia: a pragmatic
construct. Anesth Analg 1986;65:819-27. 4. Woodbridge PD. Changing concepts
concerning depth of anesthesia. Anesthesiology 1957;18:536-50. 5. Kissin
I, Gelman S. Components of anaesthesia. Br J Anaesth 1988;61:237-42. 6.
Jorgensen NH, Harders M, Hullander RM, Leivers D. Survey of preference
for spinal vs. general anesthesia: Education makes a difference. Reg Anesth
1993;18:S53. 7. Kopacz DJ, Bridenbaugh LD. Are anesthesia residency programs
failing regional anesthesia? The past, present and future. Reg Anesth 1993;18:84-87.
8. Reynolds AF, Roberts PA, Pollay M, Stratemeier PH. Quantitative anatomy
of the thoracolumbar epidural space. Neurosurgery 1985;17:905-907. 9. Westbrook
JL, Renowden SA, Carrie LES. Study of the anatomy of the extradural region
using magnetic resonance imaging. Br J Anaesth 1993;71:495-498. 10. Pitkin
GP. Controllable spinal anesthesia. Am J Surg 1928;5:537-553. 11. Koster
H. Spinal anesthesia, with special reference to its use in surgery of the
head, neck and thorax. Am J Surg 1928;5:554-570. 12. Babcock WW. Spinal
Anesthesia. An experience of twenty-four years. Am J Surg 1928;5:571-6.
13. Bromage PR. Physiology and pharmacology of epidural analgesia. Anesthesiology
1967;28:592-622. 14. Greene NM, Brull SJ. Physiology of spinal anesthesia.
Williams & Wilkins, 4th ed., 1993.
Use of Ephedrine in CSEGA
Ephedrine is the sympathomimetic drug which is most widely used to sustain
blood pressure during spinal anesthesia. The active principal was isolated
from the chinese herb ma huang in 1885 by Yamanashi (1). Butterworth et
al. (2) found that a mixed adrenergic agonist such as ephedrine more ideally
corrected the noncardiac circulatory sequelae of total spinal anesthesia
in dogs than did either a pure alpha (phenyl-ephrine) or a pure beta-adrenergic
agonist (isoproterenol). Butterworth et al. (3) also demonstrated in dogs
the effectiveness of dobutamine and dopamine as possible alternatives to
ephedrine for the pharmacologic correction of the noncardiac circulatory
sequela of total spinal anesthesia. Goertz et al. (4) investigated the
effect of ephedrine on left ventricular function in patients without cardiovascular
disease under high thoracic epidural analgesia combined with general anesthesia.
Ephedrine improved left ventricular contractility without causing relevant
changes of left ventricular afterload. 1. Goodman L, Gilman A. The pharmacological
basis of therapeutics. New York, The Macmillan Co., 1941, p.1383. 2. Butterworth
JF, Piccione Jr W, Berrizbeitia LD, Dance G, Shenim RJ, Cohn LH. Augmentation
of venous return by adrenergic agonists during spinal anesthesia. Anesth
Analg 1986;65:612-6. 3. Butterworth JF, Austin JC, Johnson MD, Berrizbeitia
LD, Dance GR, Howard G, Cohn LH. Effect of total spinal anesthesia on arterial
and venous responses to dopamine and doputamine. Anesth Analg 1987;66:209-14.
4. Goertz AW, Hubner C, Seefelder C, Seeling W, Lindner KH, Rockemann MG,
Georgieeff M. The effect of ephedrine bolus administration on left ventricular
loading and systolic performance during high thoracic epidural anesthesia
combined with general anesthesia. Anesth Analg 1994;78:101-5.
Cardiovascular effects of CSEGA
Combining epidural analgesia with general anesthesia in humans reduces
the hemodynamic demand on the heart (1-3) and provides more stable intraoperative
hemodynamics (4). In animal experiments epidural analgesia has inhibited
sympathetic coronary constriction secondary to a flow-limiting stenosis
(5), reduced infarct size (6) and reduced ST-segment changes on the electrocardiogram
in an acute coronary artery occlusion model (7). However, Mergner et al.
(8) investigated epidural analgesia combined with general anesthesia in
a swine model with a tight coronary artery stenosis. Distal to the coronary
stenosis was a moderate decrease in regional myocardial function and a
severe reduction in blood flow. The epidural analgesia reaching the level
of T1 was added to an animal which already had a decreased blood pressure
and sympathetic tone from the isoflurane/fentanyl anesthesia. No correction
of the reduced blood pressure was done in this study. Stenseth et al. (9)
investigated the cardiovascular and metabolic effects of T1-T12 epidural
block in 18 patients receiving chronic beta-adrenergic blocker medication
and scheduled for aortocoronary bypass surgery. Thoracic epidural analgesia
induced a moderate decrease in mean arterial pressure, coronary perfusion
pressure, free fatty acids and myocardial consumption of free fatty acids.
Blomberg et al. (10,11) also found no cardiac effects after a T1-T8 or
T1-T6 block in beta-adrenergic blocked patients with ischemic heart disease.
Christensen et al. (12) evaluated myocardial ischemic events by Holter
monitoring of ST-segment depression in 14 patients with angina pectoris
given spinal analgesia for minor surgery. Ephedrine in doses of 5 mg was
given, if rapid infusion of saline did not improve the arterial pressure.The
first ischemic event occurred at a mean of 338 minutes after spinal analgesia,
and not in association with the onset of block, with the decrease in mean
arterial pressure after spinal analgesia or with the administration of
ephedrine. This could be explained by increased cardiac pre- and afterload,
probably further aggravated by the volume load. 1. Baron JF, Coriat P,
Mundler O, et al. Left ventricular global and regional function during
lumbar epidural anesthesia in patients with and without angina pectoris:
influence of volume loading. Anesthesiology 1987;66:621-7. 2. Diebel LN,
Lange MP, Schneider F, et al. Cardiopulmonary complications after major
surgery: a role for epidural analgesia. Surgery 1987;102:660-6. 3. Yeager
MP, Glass DD, Neff RK, Brinck-Johnson T. Epidural anesthesia and analgesia
in high-risk surgical patients. Anesthesiology 1987;66:729-36. 4. Her C,
Kizelshteyr G, Walker V, et al. Combined epidural and general anesthesia
for abdominal aortic surgery. J Cardiothorac Anesth 1990;4:552-7. 5. Heusch
G, Deussen A, Thamer V. Cardiac sympathetic nerve activity and progressive
vasoconstriction distal to coronary stenoses: feed-back aggravation of
myocardial ischemia. J Auton Nerv Syst 1985;13:311-26. 6. Davis RF, DeBoer
LWV, Maroko PR. Thoracic epidural anesthesia reduces myocardial infarct
size after coronary artery occlusion in dogs. Anesth Analg 1986;65:711-7.
7. Vik-Mo H, Ottesen S, Renck H. Cardiac effects of thoracic epidural analgesia
before and during acute coronary artery occlusion in open-chest dogs. Scand
J Clin Lab Invest 1978;38:737-46. 8. Mergner GW, Stolte AL, Frame WB, Lim
HJ. Combined epidural analgesia and general anesthesia induce ischemia
distal to a severe coronary artery stenosis in swine. Anesth Analg 1994;78:37-45.
9. Stenseth R, Berg EM, Bjella L, Christensen O, Levang OW, Gisvold SE.
The influence of thoracic epidural analgesia alone and in combination with
general anesthesia on cardiovascular function and myocardial metabolism
in patients receiving beta-adrenergic blockers. Anesth Analg 1993;77:463-8.
10. Blomberg S, Emanuelsson H, Kvist H, et al. Effects of thoracic epidural
anesthesia on coronary arteries and arterioles in patients with coronary
artery disease. Anesthesiology 1990;73:840-7. 11. Blomberg S, Emanuelsson
H, Ricksten SE. Thoracic epidural anesthesia and central hemodynamics in
patients with unstable angina pectoris. Anesth Analg 1989;69:558-62. 12.
Christensen EF, Sogaard P, Egebo K, Bach LF, Riis J. Myocardial ischemia
and spinal analgesia in patients with angina pectoris. Br J Anaesth 1993;71:472-5.
Cord ischemia and preemptive analgesia
Breckwoldt et al. (1) investigated the effect of intrathecal tetracaine
on the neurological sequelae of spinal cord ischemia and reperfusion with
aortic occlusion in rabbits. They found that intrathecal tetracaine significantly
and dramatically abrogated the neurological injury secondary to spinal
cord ischemia and reperfusion after aortic occlusion at 30 minutes. Peripheral
tissue injury provokes two kinds of modification in the responsiveness
of the nervous system: peripheral sensitization and central sensitization.
The optimal form of pain treatment may be one that is applied both pre-,
intra-, and postoperatively to preempt the establishment of pain hypersensitivity
during and after surgery. Woolf and Chong (2) in their review of preemptive
analgesia concluded that "although evolution has conserved sensitization
in humans, the capacity to inflict `controlled injury` during surgery has
clearly not been anticipated". 1. Breckwoldt WL, Genco CM, Connolly RJ,
Cleveland RJ, Diehl JT. Spinal cord protection during aortic occlusion:
Efficacy of intrathecal tetracaine. Am Thorac Surg 1991;51:959-63. 2. Woolf
CJ, Chong MS. Preemptive analgesia - treating postoperative pain by preventing
the establishment of central sensitization. Anesth analg 1993;77:362-79.
CSEA for Cesarean section
An increasing number of parturients wish to be awake during cesarean
section (1) and opt for regional rather than general anesthesia. Spinal
block is a simple technique which requires a small dose of local anesthetic
to provide surgical anesthesia (1,2) with rapid, intense and reliable block
without missed segments (1,3), greater muscle relaxation (1) and minimal
risk of drug toxicity to the mother as well as to the fetus (3). For these
reasons it has been proposed as the anesthetic method of choice for emergent
cesarean section (4). Visceral pain is a poorly localized, dull and deep
pain which is often accompanied by nausea, vomiting and sweating. Instead
of pain, some patients describe it as a feeling of heaviness, pressure,
tightness and/or squeezing. Alahuhta et al. (5) compared the incidence
of visceral pain in 46 patients undergoing elective cesarean section under
spinal or epidural anesthesia with 0.5% bupivacaine. Visceral pain occurred
in 12/23 patients in the spinal group and in 13/23 patients in the epidural
group. Rawal et al. (1) used the combined spinal-epidural anesthesia in
15 parturients scheduled for cesarean section. With the patients in the
sitting position they injected 1.5-2 ml of 0.5% (7.5-10 mg) hyperbaric
bupivacaine through the spinal needle to achieve an S5-T8-9 block. After
withdrawing the spinal needle, the epidural needle was rotated and an epidural
catheter introduced through it. After aspiration for blood or spinal fluid,
0.5-1 ml saline was injected in the epidural catheter to test its patency.
15-20 min after the spinal injection, 0.5% plain bupivacaine 1.5-2 ml per
unblocked segment were injected till a T4-5 level was reached. The combined
mean total dose of bupivacaine was 40.2±4.24 mg. It means that only
5-7 ml of 0.5% bupivacaine injected through the epidural catheter were
needed to rise the anesthetic level from T8-9, reached by the previous
spinal injection, to T3-4 achieved by the epidural augmentation. Riley
et al. (6) compared the spinal versus epidural anesthesia for cesarean
section in relation to time efficiency. They have found that patients who
received epidural anesthesia had significantly longer total operating room
times than those who received spinal anesthesia (101 ±20 vs 83 ±16
min). This was caused by longer times spent in the operating room until
surgical incision (46 ±11 vs 29±6 min). Supplemental intraoperative
intravenous analgesics and anxiolytics were required more often in the
epidural group (38%) than in the spinal group (17%). Vucevic and Russell
(7) compared 12 ml 0.125% plain bupivacaine with 3 ml 0.5% plain bupivacaine
for cesarean section in 40 women using the combined spinal-epidural technique.
The initial spread was greater with the 12 ml solution but within 5 min
of placing the women in the supine tilted (right hip up) position, there
were no differences in the levels of sensory blockade. The study also showed
that the 12 ml solution resulted in more intensive blockade as there was
less need for extradural anesthesia in this group than in the 3 ml group.
Parturients receiving 15 mg of spinal hyperbaric bupivacaine for cesarean
delivery developed a higher mean level and longer duration of sensory analgesia
than those receiving 12 mg (8). Fan et al. (9) examined four regimens of
combined spinal-epidural anesthesia in 80 parturients for cesarean section:
1. 2.5 mg bupivacaine 0.5% intrathecally combined with 22.2±4.6
ml of lidocaine 2% epidurally. This combination provided insufficient muscle
relaxation. 2. 5 mg of bupivacaine 0.5% - spinally with 10.1 ±2.0
ml of lidocaine 2% epidurally resulted in satisfactory anesthesia with
rapid onset and minimum side effects. 3. Spinal 7.5 mg of bupivacaine 0.5%
. 4. Spinal 10 mg of bupivacaine 0.5%. Anesthesia in these groups (7.5
mg and 10 mg bupivacaine 0.5%) was mostly due to the spinal block. Their
conclusion was that the combined spinal-epidural technique, using 5 mg
of bupivacaine and with sufficient epidural lidocaine to reach a T4 level,
had the advantages of both spinal and epidural anesthesia with few of the
complications of either. Ciccozzi et al. (10) evaluated the combined spinal-epidural
anesthesia by the needle-through-needle technique in 40 parturients (20
in the sitting position and 20 in the left lateral position). Supine position
after the spinal injection was achieved in 7.5±4.3 min in the sitting
position group and in 7.7 ±4.9 min in the left lateral group. One
patient (5%) in each group received a single shot spinal because of technical
difficulties in the epidural catheter placement. Five patients (25%) of
the left lateral group showed poor spinal analgesia and then required epidural
supplementation. Mok and Tzeng (11) demonstated that 2 mg epidural morphine
combined with 30 mg ketoralac IM provided a better pain relief after cesarean
section than using the 2 mg epidural morphine alone. Swami et al. (12)
studied the effect on the blood pressure of a spinal dose of 7.5 mg vs
12.5 mg hyperbaric bupivacaine in 90 parturients for cesarean section.
Using the combined spinal-epidural technique, 23% of the 7.5 mg group needed
an epidural top-up, while none in the 12.5 mg group. Hypotension occurred
in 40% of the 12.5 mg and only in 22% of the 7.5 mg hyperbaric bupivacaine
spinal injection. Dickson and Jenkins (13) assessed the efficacy of a bolus
dose of bupivacaine 0.5% 10 ml following an infusion of 0.1% for extension
of epidural blockade for emergency cesarean section. In only 11 patients
out of 18 was the analgesic block of labour successfully converted to a
block adequate for cesarean section using 10 ml bupivacaine 0.5%. Five
patients required an additional top-up (range 3-10 ml). A general anesthetic
was necessary in two patients with blocks which had initially appeared
to be adequate. Westbrook et al. (14) induced combined spinal-epidural
anesthesia in the lateral position in 150 women presenting for cesarean
delivery. They saw CSF after the first pass of the spinal needle through
epidural needle in only 86%-92% of the time. 1. Rawal N, Schollin J, Wesstrom
G. Epidural versus combined epidural block for cesarean section. Acta Anaesthesiol
Scand 1988;32:61-6 2. Covino BG. Rationale for spinal anesthesia. International
Anesthesiology Clinics 1989;27:8-12 3. Hunt CO. Spinal anesthesia for obstetrics.
International Anesthesiology Clinics 1989;27:26-30 4. Marx GF, Lughx WM,
Cohen S. Fetal-neonatal status following Caesarean section for fetal distress.
Br J Anaesth 1984;56:1009-12 5. Alahuhta S, Kangas-Saarela T, Hollmen AI,
Edstrom HH. Visceral pain during caesarean section under spinal and epidural
anaesthesia with bupivacaine. Acta Anaesthesiol Scand 1990;34:95-98 6.
Riley ET, Cohen SE, Macario A, Desai JB, Ratner EF. Spinal versus epidural
anesthesia for cesarean section: A comparison of time efficiency, costs,
charges, and complications. Anesth Analg 1995;80:709-12 7. Vucevic M, Russell
IF. Spinal anaesthesia for Caesarean section: 0.125% plain bupivacaine
12 ml compared with 0.5% plain bupivacaine 3 ml. Br J Anaesth 1992;68:590-595
8. De Simone CA, Leighton BL, Norris MC. Spinal anesthesia for cesarean
delivery: A comparison of two doses of hyperbaric bupivacaine. Reg Anesth
1995;20:90-94 9. Fan SZ, Susetio L, Wang YP, Cheng YJ, Liu CC. Low dose
of intrathecal hyperbaric bupivacaine combined with epidural lidocaine
for cesarean section - a balance block technique. Anesth Analg 1994;78:474-7
10. Ciccozzi A, Iovinelli G, Varrassi G. Effects of posture on the spread
of local anesthetics in CSEA for Caesarean delivery. Reg Anesth 1995;20:S74
11. Mok MS, Tzeng JI. Intramuscular ketoralac enhances the analgesic effect
of low dose epidural morphine. Anesth Analg 1993;76:S269 12. Swami A, McHale
S, Abbott P, Morgan B. Low dose spinal anesthesia for cesarean section
using combined spinal-epidural (CSE) technique. Anesth Analg 1993;76:S423
13. Dickson MAS, Jenkins J. Extension of epidural blockade for emergency
Caesarean section. Anaesthesia 1994;94:636-638 14. Westbrook JL, Donald
F, Carrie LES. An evaluation of a combined spinal/epidural needle set utilising
a 26-gauge pencil point spinal needle for Caesarean section. Anaesthesia
1992;47:990-2
Corning
The first epidural anesthesia done by Corning, a New York city neurologist,
in 1885 was a "walking" epidural. He injected twice 2 ml of a 3% solution
of the hydrochlorate of cocaine into the epidural space of a man "addicted
to sexual abuse". While standing with eyes closed, the man experienced
some dizziness, but no incoordination or motor impairment was discernible
in his gait. He left the office an hour or more after the injection and
seemed "none worse for the experience" (1). 1. Marx GF. The first spinal
anesthesia: Who deserves the laurels? Reg Anesth 1994;19:429-430
Bier
August Bier (1), on August 24, 1898, asked his assistant, Dr. Hilderbrandt,
"to perform a lumbar puncture on me", 8 days after he first performed it
on a 34-year-old patient for excision of a tuberculous capsule at the ankle
joint. Bier wrote that he did not feel any discomfort "except for a quick
flash of pain in one leg at the moment that the needle penetrated the meninges".
Unfortunately, the experiment was not successful because of an error (the
syringe did not fit the needle tightly... and consequently some CSF ran
out and most of the cocaine was lost). No sensory loss ensued. Dr. Hilderbrandt
immediately offered to submit himself to the experiment, which was successful.
Both of them "went to eat after the experiments were performed on our bodies.
We had no physical discomfort, we ate, drank wine, and smoked several cigars".
However, next morning, after a one hour morning stroll Bier felt slight
headache which increased in intensity during the course of the day. Nine
days after the puncture, all the symptoms disappeared. After 3 more days,
"I was able to go on a train trip without discomfort and was fit enough
to participate in a strenuous 8 day hunting trip in the mountains". 1.
Bier AKG, von Esmarch JFA. Versuche uber Cocainisirung des Ruckenmarkes.
Dtsch Z Chir 1899;51:361-369
A new look at the lumbar extradural space pressure
The answer to the questions: Why does not the Macintosh balloon indicator
deflate, or why the hanging drop technique is unreliable was given by Shah
(1): The epidural space pressure is influenced by many factors. It is raised
by jugular venous compression, ventilation with carbon dioxide and positive
end-expiratory pressure (PEEP). The lumbar extradural pressure is increased
rapidly with stimuli known to increase CSF pressure. However, the next
question is what happens in the "normal" condition (without jugular venous
compression or CO2 inhalation, etc.)? There is a wave pressure, which is
the lumbar CSF wave pressure transmitted to the epidural space. On that
subject Shah quoted an article by Hirai et al (2) published in 1982:"The
arterial pressure wave in the spinal CSF originates from the choroid plexus...
The pulsatile vibration of the brain parenchyma derived from the blood
flow in the cerebral arteries may have enough energy to generate the spinal
CSF pulse. The amplitude of the pulse wave varies directly with intracranial
pressure". This citation is not exactly true in the light of an investigation
published by Urayama (3). He performed system analysis on 16 adult mongrel
dogs to determine the origin of the lumbar cerebrospinal fluid pulse wave.
The descending thoracic aorta was occluded to evaluate the effects of the
spinal arterial pulsations, and the thoracic aorta and inferior vena cava
were simultaneously occluded to evaluate the effects of the spinal venous
pulsations. It was concluded that, in the first harmonic wave, the components
of the lumbar cerebrospinal fluid pulse wave are as follows: spinal arterial
pulsations - 39.4%; spinal vascular (arteries and veins) pulsations - 77%;
venous pulsations in the spinal canal - 37.6%; and the intracranial pressure
pulse wave transmitted through the spinal canal from the intracranial space
to the lumbar level - 23%. So, from this investigation we can learn that
77% of the lumbar cerebrospinal fluid pulse wave which is directly transmitted
to the extradural space as an extradural pressure wave is originated in
the vascular system (arteries and veins), and not in the brain . So, any
rise in the blood pressure, which is not an infrequent observation during
epidural needle insertion, can give a concomitant rise in the extradural
pressure with the loss of the "negative" pressure in the extradural space
and "unreliable" hanging drop and Macintosh balloon indicator techniques.
1. Shah JL. Positive lumbar extradural space pressure. Br J Anaesth 1994;73:309-314.
2. Hirai O, Handa H, Ishikawa M. Intracranial pressure pulse waveform:
considerations about its origin and methods of estimating intracranial
pressure dynamics. Brain Nerve (Tokyo) 1982;34:1059-1065. 3. Urayama K.
Origin of lumbar cerebrospinal fluid pulse wave. Spine 1994;19:441-445
Do not rotate the epidural needle
The epidural needle rotation in CSEA using the needle-through-needle
technique was first suggested in 1988 by Rawal et al. (1). However, Dr.
Rawal abandoned this technique of epidural needle rotation (2) because
he was convinced that "180° rotation of the epidural needle may cause
dural tear". Nickalls and Dennison (3) found that the distance the spinal
needle has to be advanced past the end of the Tuohy needle to just puncture
the dura ranges from 0.3 to 1.05 cm. Joshi and McCarroll (4) described
two sets of needle-through-needle techniques to perform the combined spinal-epidural
anesthesia. They were concerned to find cerebrospinal fluid in the Tuohy
needle after removal of the spinal needle. Carter et al. (5) abandoned
this technique of epidural needle rotation because it increased the chance
of inadvertent dural puncture by a factor of 5.6: there was also a 16.6%
incidence of the epidural catheter protruding through the hole made previously
by the spinal needle. Meiklejohn (6) found that "postmortem dura mater
demonstrated that rotation of the epidural needle significantly decreases
the force required to puncture the dura". He concluded that "once the needle
has been inserted into the epidural space... it should not be moved for
any reason other than to remove it". 1. Rawal N, Schollin J, Wesstrom G.
Epidural versus combined spinal epidural block for cesarean section. Acta
Anaesthesiol Scand 1988;32:61-6 2. Rawal N. Combined spinal-epidural needle
(CSEN) for the combined spinal-epidural block - reply. Acta Anaesthesiol
Scand 1989;33:618 3. Nickalls RWD, Dennison B. A modification of the combined
spinal and epidural technique. Anaesthesia 1984;39:935 4. Joshi GP, McCarroll
SM. Combined spinal-epidural anesthesia using needle-through-needle technique.
Anesthesiology 1993;78:406-7 5. Carter LC, Popat MT, Wallace DH. Epidural
needle rotation and inadvertent dural puncture with catheter. Anaesthesia
1992;47:447-8 6. Meiklejohn BH. The effect of rotation of an epidural needle.
Anaesthesia 1987;42:1180-2
Epidural rostral augmentation of spinal anesthesia
Suzuki et al. (1) found that spinal puncture with a 26G spinal needle,
with no spinal anesthetic injection, immediately before epidural injection
of 18 ml 2% mepivacaine resulted in rapid caudal spread of analgesia as
compared to an epidural anesthesia alone. They attributed it to the flow
of local anesthetic into the subarachnoid space through the perforation
produced by the spinal needle. Dobson et al. (2) reported of a sudden asystole
70 min after intrathecal injection of 2.75 ml hyperbaric bupivacaine 0.5%
in a patient whose cardiac output was being monitored. After successful
resuscitation , the height of the block was judged to be T4. According
to the authors of the report, monitoring should continue for at least 90
min after induction of spinal anesthesia. Bodily et al. (3) warned that
changes in position can alter the spread of sensory blockade for at least
1 hr after the intrathecal injection of a hypobaric solution. They showed
that 8 ml lidocaine 0.5% (baricity 0.9985±0.0003, 25°C) produced
effective spinal anesthesia for perirectal surgery in the jack-knife position.
Dermatomal levels remained low (T11-L5) while the patients were in the
head-down position during surgery, but rose two to six dermatomes if the
patient`s head was elevated after surgery. Fast rate of injection (0.5
ml/sec) of 5 ml 0.3% bupivacaine into the subarachnoid space results in
a higher maximum sensory level than slow rate injection (0.02 ml/sec) (4).
Serpell et al. (5) recorded intrathecal pressure after instillation of
saline boluses into the epidural space in adult ewes. Mean baseline CSF
pressure was 28.5±5.5 mmHg. Five ml saline boluses (1 ml/sec) were
injected at 5-minute intervals until CSF pressure exceeded 100 mmHg. Initially,
a rapid increase in CSF pressure accompanied each saline bolus with a gradual
return to baseline. Up to a cumulative volume of 20 ml (range 5-60), the
mean value of peak CSF pressure was 53±12 mmHg and the resting pressure
would return to baseline. After a cumulative injection volume of 50.5±39.5
ml (range 15-115) saline, the resting pressure progressively rose to 64.1
±17.4 mmHg to coincide with a peak CSF pressure exceeding 100 mmHg,
indicating that the compliance of the spinal space had been compromised.
Radiographic contrast injected into the caudal sheath revealed that initial
decompression occurred via leakage into the large sacral root foramina
and sheaths. Dell and Orlikowski (6) described a 26-year-old patient who
received 45 ml of bupivacaine 0.25% (including a 3 ml of bupivacaine 0.5%
as a test dose) within 3 hours of labour analgesia. One hour after the
last dose of epidural bupivacaine, with the patient in the left lateral
position, 2.5 ml of hyperbaric bupivacaine 0.5% was injected through a
25 gauge Whitacre needle into the subarachnoid space for cesarean section,
because the epidural sensory block was patchy. Two minutes later, there
was profound motor block of the lower limbs. At 5 min she developed paresthesias
and weakness in the upper limbs and experienced difficulty in breathing.
At 8 min she complained of nasal stuffiness and her trachea was intubated
following rapid sequence induction of general anesthesia. The reduced CSF
volume following epidural injection of a relatively large volume (45 ml)
was suggested as an explanation for this high spinal anesthesia following
2.5 ml hyperbaric bupivacaine spinal injection. D`Angelo et al. (7) found
a rapid cephalad spread of intrathecal sufentanil 10 æg combined
with 12 ml epidural saline injection for labor analgesia. However, they
have "blamed" this phenomenon only on the opioid pharmacokinetics and not
the epidural saline rostral augmentation of intrathecal sufentanil. Barclay
et al. (8) showed that compression of the vena cava by an abdominal binder
decreases the volume of the subarachnoid space and heightens the level
of spinal anesthesia. Furst and Reisner (9) described two cases of high
spinal anesthesia following failed epidural blockade. They found its incidence
to be 11% versus fewer than 1% in patients undergoing spinal anesthesia
alone. In light of these findings, they changed their practice by reducing
the dose of spinal bupivacaine by 20% in those patients in whom epidural
anesthesia has proved inadequate. They also perform the spinal block in
the sitting position, allowing it to "set" for 60-90 seconds prior to placing
the patient supine. Gamil (10) reported a case of a parturient for cesarean
section who received spinal anesthesia with 2.5 ml of 0.5% heavy bupivacaine
in the sitting position. The patient was maintained in this position whilst
an epidural catheter was sited in a cephalad direction. It took 15 min.
Before threading the epidural catheter, the epidural space was primed with
20 ml of saline. Then the patient positioned for surgery, supported under
the shoulders by three pillows. 75 min from the insertion of the spinal,
at the end of surgery, 50 ml of saline was injected to the epidural space
as prophylaxis against headache. 5 min later the block extended from L1
to T1. The injection of a relatively small amount of 0.5% bupivacaine into
the extradural space after a subarachnoid injection of a standard dose
of bupivacaine results in rapid extension of the block (11,12). Several
hypotheses have been advanced to explain this enhancement of the subarachnoid
block. These include leakage of extradural bupivacaine into the subarachnoid
space via the hole created by the subarachnoid puncture, the existence
of a "subclinical" analgesia at a higher level which is enhanced and becomes
evident by perineural or transdural spread of the extradural solution,
or the continuing spread of the initial subarachnoid injection independent
of the extradural injection (11-14). Blumgart et al. (15) found that the
mechanism of extension of spinal anesthesia by extradural injection of
local anesthetics is largely a volume effect. Using extradural saline 10
ml and extradural bupivacaine 0.5% 10 ml - the extension of the block was
found to be similar in the saline or the bupivacaine groups and significantly
faster than the group which received no extradural injection after spinal
injection of 1.6-1.8 ml of 0.5% hyperbaric bupivacaine. 1. Suzuki N, Koyanemaru
M, Onizuka S, Takasaki M. Dural puncture with a 26-gauge spinal needle
affects epidural anesthesia. Reg Anesth 1995;20:S118 2. Dobson PMS, Caldicott
LD, Gerrish SP. Delayed asystole during spinal anaesthesia for transurethral
resection of the prostate. Eur J Anaesth 1993;10:41-43 3. Bodily MN, Carpenter
RL, Owens BD. Lidocaine 0.5% spinal anaesthesia: A hypobaric solution for
short-stay perirectal surgery. Can J Anaesth 1992;39:770-773 4. Horlocker
TT, Wedel DJ, Wilson PR. Effect of injection rate on sensory level and
duration of hypobaric bupivacaine spinal anesthesia for total hip arthroplasty.
Anesth Analg 1994;79:773-7 5. Serpell MG, Coombs DW, Colburn RW, Deheo
JA, Twitchell BB. Intrathecal pressure recordings due to instillation in
the epidural space. International Monitor on Regional Anaesthesia 1993;52
6. Dell RG, Orlikowski CEP. Unexpectedly high spinal anaesthesia following
failed extradural anaesthesia for caesarean section. Anaesthesia 1993;48:641
7. D`Angelo R, Anderson MT, Philip J, Eisenach JC. Intrathecal sufentanil
compared to epidural bupivacaine for labor analgesia. Anesthesiology 1994;80:1209-1215
8. Barclay DL, Renegar OJ, Nelson EW. The influence of inferior vena cava
compression on the level of spinal anesthesia. Am J Obstet Gynecol 1968;101:792-800
9. Furst SR, Reisner LS. Risk of high spinal anesthesia following failed
epidural block for cesarean delivery. J Clin Anesth 1995;7:71-74 10. Gamil
M. Combined spinal/epidural anaesthesia for caesarean section. Anaesthesia
1994;49:545-6 11. Carrie LES. Epidural versus combined spinal epidural
block for Caesarean section. Acta Anaesthesiol Scand 1988;32:595-596 12.
Rawal N, Schollin J, Wesstrom G. Epidural versus combined spinal epidural
block for Caesarean section. Acta Anaesthesiol Scand 1988;32:61-66 13.
Rawal N. Single segment combined subarachnoid and epidural block for Caesarean
section. Can Anaesth Soc J 1986;33:254-255 14. Bromage PR. Mechanism of
action of extradural anaesthesia. Br J Anaesth 1975;47:199-212 15. Blumgart
CH, Ryall D, Dennison B, Thompson-Hill LM. Mechanism of extension of spinal
anaesthesia by extradural injection of local anaesthetic. Br J Anaesth
1992;69:457-460
Metallic particles in the needle-through-needle technique
The Tuohy needle was not originally intended to be an introducer for
a spinal needle. Tuohy (1) in 1944, used a needle with a curved Huber tip
for continuous spinal anesthesia, and Curbelo (2) in 1949, adapted this
needle for continuous epidural block. Coates (3) and Mumtaz et al. (4)
were the first to publish the possibility of inserting a long spinal needle
through a Tuohy epidural needle. They encountered only two potential hazards,
"possible passage of the epidural catheter through the hole in the dura
mater and the possibility of subarachnoid effects from epidurally injected
drugs by passage through the hole in the dura". Evans (5) applied for a
patent for this instrument a year later. The long spinal needles have been
available in the British market since 1985 (6). The forward end of the
spinal needle is inclined at an angle of about 30° to its length when
it projects by about 10 mm from the forward end of the epidural needle
(5). At that inclination the spinal needle scratches the inner surface
of the epidural needle tip when moving forward and backward. This friction
must cause metallic microparticles. Spectral analysis of the 18-gauge epidural
needle (Portex) at 20 KV (7) revealed 18.96±0.28% chromium and 68.75
±0.82% iron. The other components were: nickel, 9.35±0.57%;
manganese, 1.85 ±0.07%; silicone, 0.67±0.16%; and molybdenum,
0.31 ±0.23%. For example, nickel implanted in rats produced a necrotic,
abcesslike reaction (8). In the clinical setting, an epidural catheter
is pushed through the shaft after the spinal needle is withdrawn, so the
microparticles produced by the friction between the two needles can be
pushed forward by the force exerted to insert the catheter into the epidural
space. 1. Tuohy EB. Continuous spinal anesthesia: Its usefulness and technique
involved. Anesthesiology 1944;5:142-143 2. Curbelo MM. Continuous peridural
segmental anesthesia by means of a ureteral catheter. Curr Res Anesth Analg
1949; 28:13 3. Coates MB. Combined subarachnoid and epidural techniques.
Anaesthesia 1982;37:89-90 4. Mumtaz MH, Daz M, Kuz M. Another single space
technique for orthopaedic surgery. Anaesthesia 1982;37:90 5. Evans JM.
Instrument for epidural and spinal anaesthesia: UK patent application,
1983: GB 2124503A 6. Desira WR. A special needle for combined subarachnoid
and epidural block. Anaesthesia 1984;39:308 7. Kumar B, Messahel FM. Evaluation
of epidural needles. Acta Anaesthesiol Scand 1987;31:96-99 8. Wigle RL.
The reaction of copper and other projectile metals in body tissues. J Trauma
1992;33:14-18
Superselective spinal anesthesia
Veneziani et al. (1) described a technique of superselective spinal
anesthesia for the surgical treatment of saphenectomy. The block has been
performed at L2-3 with the patients laying in omolateral decubitus with
respect to surgical side and injecting slowly 1% hyperbaric bupivacaine
0.5-0.6 ml and maintaining such a position for about 10-15 minutes. The
24G Sprotte spinal needle was used with an incidence of only 0.4% postspinal
headache. 1. Veneziani A, Santagostino G, Matera D, Tulli G. Superselective
spinal anaesthesia for the surgical treatment of saphenectomy. Acta Anaesthesiol
Scand 1995;39:A430
CSEA in uncommon disease
Cherng et al. (1) described a case report of combined spinal and epidural
anesthesia for abdominal hysterectomy in a 34-year-old woman with myotonic
dystrophy. Patients with myotonic dystrophy have a high risk of anesthetic
complications, and the anesthetic technique should aim to prevent any stimulation
(chemical, mechanical or thermal), and avoid any drugs that would induce
uncontrollable muscular contraction (myotonic crisis) (2). 1. Cherng YG,
Wang YP, Liu CC, Shi JJ, Huang SC. Combined spinal and epidural anesthesia
for abdominal hysterectomy in a patient with myotonic dystrophy. Reg Anesth
1994;19:69-72 2. Paterson RA, Tousignant M, Skene DS. Caesarean section
for twins in a patient with myotonic dystrophy. Can Anaesth Soc J 1985;32:418-421
CSEA for laparoscopic operations
Ciofolo et al. (1) evaluated the respiratory effects of laparoscopy
under epidural anesthesia in seven female patients scheduled for a gamete
intrafallopian transfer procedure. No significant changes in the ventilatory
variables were observed in the Trendelenburg position. In contrast, CO2
insufflation significantly increased minute ventilation (from 9.1±1.0
L/min to 11.8 ±2.6 L/min) and respiratory rate (from 16.9±1.9
breaths/min to 23.1 ±3.3 breaths/min), whereas CO2 output remained
unchanged. PaCO2 remained constant throughout the study. They concluded
that epidural anesthesia may be a safe alternative to general anesthesia
for outpatient laparoscopy, as it is not associated with ventilatory depression.
Epidural analgesia for minilaparotomy cholecystectomy improves pain relief
in the immediate postoperative period, compared to intramuscular morphine
(2). Reduction of the surgical stress response can be achieved by two techniques:
One is to reduce the degree of tissue trauma and thereby the injury response
using the "minimal invasive surgery concept"; the other is "stress-free
anesthesia and surgery" providing effective pain relief, including afferent
neural block (3,4), together with block of various humoral mediator cascade
systems (arachidonic cascade metabolites, cytokines, etc.) as well as a
maintenance of nutritional status by provision of unspecific nutrients
(glutamine, arginine) or growth factors (growth hormone, etc.) (5). 1.
Ciofolo MJ, Clergue F, Seebacher J, Lefebvre G, Viars P. Ventilatory effects
of laparoscopy under epidural anesthesia. Anesth Analg 1990;70:357-61 2.
Dahl JB, Hjortso N-C, Stage JG, Hansen BL, Moiniche S, Damgaard B, Kehlet
H. Effects of combined perioperative epidural bupivacaine and morphine,
ibuprofen, and incisional bupivacaine on postoperative pain, pulmonary,
and endocrine-metabolic function after minilaparotomy cholecystectomy.
Reg Anesth 1994;19:199-205 3. Kehlet H. Modification of responses to surgery
and anesthesia by neural blockade: Clinical implications. In:Cousins MJ,
Bridenbaugh PO, eds. Neural blockade in clinical anesthesia and management
of pain. Philadelphia, Lippincott, 1987:145-188 4. Kehlet H. General vs
regional anesthesia. In: Rogers MC, Tinker JH, Covino EG, Longnecker DE
(eds.). Principles and practice of anesthesiology. St Louis, C.V. Mosby,
1993:1218-1234 5. Kehlet H. Postoperative pain relief. A look from the
other side. Reg Anesth 1994;19:369-377
Postoperative epidural analgesia
Albert Schweitzer said that "pain is a more terrible lord of mankind
than even death itself". Bonica (1) wrote that "acute and chronic pain
afflicts millions upon millions of persons annually, and in many patients
with chronic pain and a significant percentage of those with acute pain,
it is inadequately relieved". In the 1980s, surveys of patients` subjective
well-being revealed an incidence of moderate or severe pain after surgery
of 31-75% (2,3). De Leon-Casasola et al. (4) compared the effect on postoperative
myocardial ischemia of epidural versus intravenous patient-controlled analgesia.
198 patients received either technique for 5-7 days postoperatively. Patients
in the epidural group had a lower incidence of tachycardia (14% vs. 65%),
ischemia (5% vs. 17%), and infarction - 0% vs. 20% of patients with ischemia
in the intravenous patient-controlled analgesia group. Postoperative ileus
is an undesirable response to injury and is predominantly caused by an
increase in inhibitory afferent sympathetic activity (5). Postoperative
continuous epidural analgesia may improve gastrointestinal motility and
reduce ileus (6-9). Early oral feeding reduced the risk of septic complications
(10). The positive effect of epidural local anesthetic analgesic techniques
on gastrointestinal paralysis may facilitate early oral nutrition as well
as reducing fatigue and convalescence. 1. Bonica J.J. History of pain concepts
and pain therapy. Mt Sinai J Med 1991;58:191-202 2. Kuhn S, Cooke K, Collins
M, Jones JM, Mucklow JC. Perceptions of pain relief after surgery. Br Med
J 1990;300:1687-1690 3. Owen H, McMillan V, Royowski D. Postoperative pain
therapy: A survey of patients` expectations and their experiences. Pain
1990;41:303-307 4. De Leon Casasola OA, Lema MJ, Karabella D, Harrison
P. Postoperative myocardial ischemia: Epidural versus intravenous patient-controlled
analgesia. Reg Anesth 1995;20:105-112 5. Wattwill M. Postoperative pain
relief in gastrointestinal motility. Acta Chir Scand 1988;550(Suppl):140-145
6. Bredtmann RD, Herden RN, Teichmann W, Moecke HP, Kniesel B, Batdgen
R, Tecklenburg A. Epidural analgesia in colonic surgery: Results of a randomized
prospective study. Br J Surg 1990;77:638-642 7. Sheinin B, Asantila R,
Orku R. The effect of bupivacaine on pain and bowel function after colonic
surgery. Acta Anaesthesiol Scand 1987;31:161-164 8. Ahn H, Bronge A, Johansson
K, Ygge H, Lindhargen J. Effect of continuous postoperative epidural analgesia
on intestinal motility. Br J Surg 1988;75:1176-1178 9. Wattwill M, Thoren
T, Hennerdal S, Garvill J-E. Epidural analgesia with bupivacaine reduces
postoperative paralytic ileus after hysterectomy. Anesth Analg 1989;68:353-358
10. Moore FA, Philiciano DV, Andrassy REJ, McArdle AH, Booth FVM, Morgenstein-Wargnen
TB, Kellum JM, Welling RE, Moore EE. Early enteral feeding, compared with
parenteral, reduces postoperative septic complications: The results of
a meta-analysis. Ann Surg 1992;216:172-183
Unilateral spinal anesthesia
Using the needle-through-needle technique in 80 patients for cesarean
section Fan et al. (1) noted the occurrence of a unilateral spinal block
with the hyperbaric 0.5% bupivacaine, "because keeping the patient in the
lateral position was necessary to accomplish the epidural procedure". 1.
Fan SZ, Susetio L, Wang YP, Cheng YJ, Liu CC. Low dose of intrathecal hyperbaric
bupivacaine combined with epidural lidocaine for cesarean section - a balance
block technique. Anesth Analg 1994;78:474-7
CSEA for abdominal operations
Guedj et al. (1) compared between spinal anesthesia and combined spinal-epidural
anesthesia (CSEA) in 63 patients undergoing gynecological surgery. Spinal
anesthesia (n=34) was carried out in the L3-4 interspace with the patients
sitting using 15 mg of hyperbaric 0.5% bupivacaine with adrenaline. In
the CSEA group (n=29) an epidural catheter was inserted through the L2-3
interspace and the spinal anesthesia in the L3-4 interspace, while the
patients were sitting. In the CSEA group, excellent analgesia was obtained
in all patients. In the spinal group, general anesthesia was required in
3 patients (8.8%), as anesthesia only reached the T12 level in 2 cases,
and as surgery lasted longer than the spinal in the third one. Moiniche
et al. (2) described a case of colonic resection with early discharge after
combined subarachnoid - epidural analgesia, preoperative glucocorticoids,
and early postoperative mobilization and feeding in a 59-year-old pulmonary
high-risk woman. They have introduced an epidural catheter between T9-10
and a spinal catheter between L3-4. During the operation the patient was
fully awake. At one time during intestinal traction, visceral pain was
treated vith intravenous 100 æg fentanyl. Surgery lasted for 70 minutes.
The spinal catheter was removed at the end of surgery, while the epidural
catheter provided postoperative analgesia for 72 hours. Luchetti et al.
(3) used the combined spinal-epidural anesthesia in 20 patients undergoing
surgery for hernioplasty, saphenectomy, hemorroidectomy and varicocelectomy.
The subarachnoid injection consisted of hyperbaric bupivacaine 1% 1 ml
and the epidural catheter injection - bupivacaine 0.5% 3 ml + fentanyl
50 µg. Analgesia was excellent in 17 patients and good in 3. No patient
needed further analgesic medication intraoperatively. Mihic and Abram (4)
compared five groups of patients undergoing abdominal hysterectomy with
or without appendicectomy with regional anesthesia. Two hundred patients
were divided as follows: Group 1 - spinal anesthesia with hyperbaric 0.5%
bupivacaine; Group 2 - as group 1 with the addition of 0.06 mg of IV buprenorphine
and 2.5 mg of IV midazolam; Group 3 - epidural block with 0.75% bupivacaine;
Group 4 - as group 3 with the addition of epidural morphine 1%; Group 5
- combined spinal-epidural block (as in groups 1 and 4). No case of unsuccessful
blockade occurred in the combined spinal-epidural anesthesia, compared
to 3-4 cases of failed block in the other groups. Four patients whose analgesia
was considered to be unsuccessful had to be intubated to obtain satisfactory
surgical conditions. The combination of subarachnoid and epidural block
provided the best analgesia. 1. Guedj P, Eldor J, Gozal Y. Conventional
spinal block versus combined spinal-epidural anaesthesia for lower abdominal
surgery. Ann Fr Anesth Reanim 1992;11:399-404 2. Moiniche S, Dahl JB, Rosenberg
J, Kehlet H. Colonic resection with early discharge after combined subarachnoid-epidural
analgesia, preoperative glucocorticoids, and early postoperative mobilization
and feeding in a pulmonary high-risk patient. Reg Anesth 1994;19:352-356
3. Luchetti M, Palomba R, Liardo A, Bardari G, Sica G. Combined spinal-epidural
anaesthesia (CSEA) is effective and safe for minor general surgery. Int
Monitor Reg Anaesth 1994;A97 4. Mihic DN, Abram SE. Optimal regional anaesthesia
for abdominal hysterectomy: Combined subarachnoid and epidural block compared
with other regional techniques. Eur J Anaesthesiol 1993;10:297-301
CSEA for thoracic operations
Kowalewski et al. (1) reported on the use of spinal anesthesia with
hyperbaric bupivacaine (20-30 mg) and/or lidocaine (150 mg) with morphine
(0.5-1 mg) combined with general anesthesia with alfentanil 97 ±22
µg/Kg and midazolam 0.04±0.02 mg/Kg supplemented with a muscle
relaxant and maintained with isoflurane (0.25-0.5%) in oxygen in 18 patients
for coronary artery bypass surgery (CABG). They suggested that general
anesthesia combined with spinal anesthesia may be an effective technique
for CABG. Very low concentrations of inhalational agents are required to
maintain unconsciousness during high spinal anesthesia (2). Epidural anesthesia
attenuates the endocrine-metabolic responses to surgical stress (3), reduces
intestinal paralysis (4,5) and decreases perioperative morbidity (6,7).
Thoracic epidural anesthesia decreases heart rate, mean arterial pressure,
cardiac output and left ventricular contractility (8,9). Dopamine effectively
counters cardiovascular depression during thoracic epidural anesthesia
(10,11). Dopamine effectively and dose-dependently counters cardiovascular
depression induced by the anesthetic technique of combining isoflurane
and thoracic epidural anesthesia (12). Animals` experiments demonstrated
that spinal cord section (13) or its cooling at the T1 level (14) resulted
in behavioral and electrophysiological evidence of sleep. Subarachnoid
bupivacaine blockade decreased the hypnotic dose of thiopental from 3.40
±0.68 mg/Kg to 2.17±0.48 mg/Kg. The ED50 value of midazolam
also decreased with bupivacaine blockade, from 0.23 mg/Kg to 0.06 mg/Kg.
It was suggested that the reduction in hypnotic requirements was due to
the decrease in afferent input induced by spinal anesthesia (15). Extension
of the segmental block to involve the cardioaccelerator fibers (above T4)
is commonly advanced as a reason to explain the bradycardia that may accompany
epidural analgesia (16), however, central volume depletion may have a greater
cardioinhibitory vasodepressor influence (16,17). 1. Kowalewski RJ, MacAdams
CL, Eagle CJ, Archer DP, Bharadwaj B. Anaesthesia for coronary artery bypass
surgery supplemented with subarachnoid bupivacaine and morphine: a report
of 18 cases. Can J Anaesth 1994;41:1189-95 2. Greene NM, Brull SJ. Physiology
of spinal anesthesia. 4th ed. Baltimore: Williams & Wilkins, 1993:61-8
3. Kehlet H. Modification of responses to surgery by neural blockade: clinical
implications. In: Cousins MJ, Bridenbaugh PO, eds. Neural bloclkade. Philadelphia:
JB Lippincott, 1988:145-188 4. Scheinin B, Asantila R, Orko R. The effect
of bupivacaine and morphine on pain and bowel function after colonic surgery.
Acta Anaesthesiol Scand 1987;31:161-164 5. Ahn H, Bronge A, Johansson K,
Ygge H, Lindhagen J. Effect of continuous postoperative epidural analgesia
on intestinal motility. Br J Surg 1988;75:1176-1178 6. Yeager MP, Glass
DD, Neff RK, Brinck-Johnson T. Epidural anesthesia and analgesia in high-risk
surgical patients. Anesthesiology 1987;66:729-736 7. Scott NB, Kehlet H.
Regional anaesthesia and surgical morbidity. Br J Surg 1988;75:299-304
8. Reiz S, Nath S, Ponten E, Friedman A, Backlund U, Olsson B, Rais O.
Effects of thoracic epidural block and the beta-1-adrenoreceptor agonist
prenalterol on the cardiovascular response to infrarenal aortic cross-clamping
in man. Acta Anaesthesiol Scand 1979;23:395-403 9. McLean APH, Mulligan
GW, Otton P, MacLean LD. Hemodynamic alterations associated with epidural
anesthesia. Surgery 1967;62:79-87 10. Lundberg J, Biber B, Henriksson BA,
Martner J, Raner C, Werner O, Winso O. Effects of thoracic epidural anesthesia
and adrenoreceptor blockade on the cardiovascular response to dopamine
in dog. Acta Anaesthesiol Scand 1991;35:359-365 11. Lundberg J, Norgren
L, Thomson D, Werner O. Hemodynamic effects of dopamine during thoracic
epidural analgesia in man. Anesthesiology 1987;66:641-646 12. Raner C,
Biber B, Lundberg J, Martner J, Winso O. Cardiovascular depression by isoflurane
and concomitant thoracic epidural anesthesia is reversed by dopamine. Acta
Anaesthesiol Scand 1994;38:136-143 13. Ho T, Wang YR, Lin TAN, Chang YF.
Predominance of electrocortical sleep patterns in the "encephale isole"
cat and new evidence for a sleep center. Physiol Bohemosloven 1960;9:85-92
14. Oreshchuk FA. The development of sleep on local cooling of the spinal
cord. Fiziol Z (Moscow) 1960;46:1230-5 15. Tverskoy M, Shagal M, Finger
J, Kissin I. Subarachnoid bupivacaine blockade decreases midazolam and
thiopental hypnotic requirements. J Clin Anesth 1994;6:487-490 16. Bromage
PR. Physiology and pharmacology of epidural anesthesia. Anesthesiology
1967;28:592-608 17. Arndt JO, Hock A, Stanton Hicks M, Stuhmeier KD. Peridural
anesthesia and the distribution of blood in supine humans. Anesthesiology
1985;63:616-623
Anesthetic risk factors
In a survey among 1,152 Australian and New Zealand anesthetists Kitching
et al. (1) evaluated the percentage of anesthetists who warn patients before
operation about "material risks" like death, neurological injury, awareness,
failed intubation, failed block, seizures, etc. Only 1-9% have discussed
and documented these items to their patients. 55% discussed but not documented
the subject of failed block compared to 2% - for failed intubation. 36-97%
did not discuss these matters at all pre-operatively. 1. Kitching A, Love
J, Donnan G. Mishap or negligence. Br J Anaesth 1995;74:110-111
Medico-legal aspects of CSEA
Reports of cauda equina syndrome associated with micro-bore spinal catheter
use, resulted in their removal from clinical practice in the USA (1). Finucane
(2) in an editorial on the dosage dilemma of spinal anesthesia for cesarean
delivery wrote that "the era of the microcatheter technique was short lived...
The combined spinal-epidural technique is an excellent alternative and
addresses many of the issues raised. One does not have to commit to a large
initial subarachnoid dose of local anesthetic, supplementation may be administered
epidurally, and opioids may be administered in this fashion for postoperative
pain relief". 1. FDA Safety Alert; 29.5.92 2. Finucane BT. Spinal anesthesia
for cesarean section: The dosage dilemma. Reg Anesth 1995;20:87-89
Spinal opioid pruritus and emesis
Larger doses of spinal morphine result in a greater incidence of pruritus
(1). Knudsen and Lisander (2) decreased the incidence of emesis post subarachnoid
morphine from 58% to 17% by 20 mg metoclopramide given intramuscularly
before and after the surgery. Combined use of intrathecal sufentanil and
bupivacaine can reduce the incidence of pruritus due to the sole use of
intrathecal sufentanil for labor analgesia. Abouleish et al. (3) used spinal
injection of bupivacaine 2.5 mg and sufentanil 10 µg in the combined
spinal-epidural analgesia (CSEA) and found an incidence of 21%. However,
D`Angelo et al. (4) used only intrathecal sufentanil 10 µg in CSEA
with an incidence of pruritus of 84%. 1. Fuller JG, McMorland GH, Douglas
MJ, Palmer L. Epidural morphine for analgesia after caesarean section:
A report of 4880 patients. Can J Anaesth 1990;37:636-40 2. Knudsen K, Lisander
B. Metoclopramide decreases emesis after spinal anesthesia supplemented
with subarachnoid morphine. Reg Anesth 1994;19:390-394 3. Abouleish A,
Abouleish E, Camann W. Combined spinal-epidural analgesia in advanced labour.
Can J Anaesth 1994;41:575-8 4. D`Angelo R, Anderson MT, Philip J, Eisenach
JC. Intrathecal sufentanil compared to epidural bupivacaine for labor analgesia.
Anesthesiology 1994;80:1208-1215
Endocrine responses to spinal or epidural anesthesia
The endocrine response measured by plasma cortisol and glucose levels
was not abolished by thoracic epidural etidocaine (1). Studies have failed
to dampen the endocrine metabolic response to surgical trauma by thoracic
epidural anesthesia unless this has been combined with spinal anesthesia
(2). 1. Dahl JB, Rosenberg J, Kehlet H. Effect of thoracic epidural etidocaine
1.5% on somatosensory evoked potentials, cortisol and glucose during cholecystectomy.
Acta Anaesthesiol Scand 1992;36:378-382 2. Dahl JB, Rosenberg J, Dirkes
WE, Mogensen T, Kehlet H. Prevention of postoperative pain by balanced
analgesia. Br J Anaesth 1990;64:518-520
Epidural unilateral blockade
The incidence of unilateral blockade in continuous lumbar epidural anesthesia
is 5.9% (1). There have been four etiologic factors described for the development
of unilateral epidural blockade (2-9):1. Slow injection of small volumes,
patient position, and baricity of local anesthetic solution may cause anesthetic
solutions to pool on the lower side during injection; 2. A congenital median
epidural septum or acquired midline adhesion may act as a diffusion barrier;
3. The epidural catheter tip may pass through an intervertebral foramen
resulting in production of a unilateral paravertebral block; 4. The epidural
catheter tip may be in the anterior epidural space resulting in longitudinal
and ipsilateral transverse spread of local anesthetics, instead of circumferential
spread around the dura. Unilateral epidural block is more common in women
receiving repeat epidurals (6.6% vs. 18.3%) (10). Crawford (11) reported
an incidence of two cases of inadequate epidural block (one unilateral
block; one missed segment) in 17 women who received epidural analgesia
after a blood patch. In a further woman the sensory level could not be
extended above T10 for cesarean section. 1. Asato F, Hirakawa N, Oda M,
Iyatomi I, Nagasawa I, Katekawa Y, Totoki T. A median epidural septum is
not a common cause of unilateral epidural blockade. Anesth Analg 1990;71:427-9
2. Singh A. Unilateral epidural analgesia. Anaesthesia 1967;22:147-9 3.
Shanks CA. Four cases of unilateral epidural analgesia. Br J Anaesth 1968;40:999-1002
4. Usubiaga JE, Dos Reis A, Usubiaga LE. Epidural misplacement of catheters
and mechanisms of unilateral block. Anesthesiology 1970;32:158-61 5. Bozeman
PM, Chandra P. Unilateral analgesia following epidural and subarachnoid
block. Anesthesiology 1980;52:356-7 6. De Rosayro AM. A case of unilateral
analgesia following epidural and subarachnoid block revisited. Anesthesiology
1981;55:478 7. Bailey PW. Median epidural septum and multiple cannulation.
Anaesthesia 1986;41:881-2 8. Nunn G, Mackinnon RP. Two unilateral epidural
blocks. Anaesthesia 1986;41:439-40 9. Hehre FW, Sayig JM, Lowman RM. Etiologic
aspects of failure of continuous lumbar peridural anesthesia. Anesth Analg
1960;39:511-7 10. Withington DE, Weeks SK. Repeat epidural analgesia and
unilateral block. Can J Anaesth 1994;41:568-71 11. Crawford SJ. Epidural
blood patch. Anaesthesia 1985;40:381
Combined spinal-epidural anesthesia: The anesthesia of choice
In 1992 (1) only 6.6% of patients operated in 17 European countries
received epidural or spinal opioid analgesia. 89.2% received epidural opioids,
while 10.8% intrathecal opioids (ratio 8:1). In a recent review on regional
anesthesia and analgesia for same-day surgery in adults Wurm (2) stated
that "regional anesthesia continuous to remain under-utilized for same-day
surgery. Reasons for this include uncertainty of success, prolonged preparation
time, and special skills required by the anesthesiologist". Lyons et al.
(3) found a "demonstrable lack of enthusiasm for the sequential separate
punctures amongst women who had previous experience of regional anesthesia
for caesarean section. An additional skin breech, while seeming trivial
in itself, may have had a greater impact on patient acceptance". There
is a considerable variation in the frequency with which regional anesthesia
is used. A review of 6,000 patients at the Royal Adelaide Hospital revealed
that only 3% received regional anesthesia (4). In contrast, in a review
of 1-year prospective analysis (5), the Hospital for Special Surgery in
New York City used regional anesthesia in 89% of their orthopedic outpatient
population. The incidence of spinal anesthesia in an orthopedic institute
in Firenze increased from 22% in 1989 to 42% in 1993 (6). However, the
incidence of epidural anesthesia decreased from 20% to 4% during that period.
The overall incidence of regional anesthesia (spinal and epidural) increased
only in 2%. This was due to the introduction of the 25G Quincke needle
in 1990, and the blunting needles in 1993 (Sprotte 24G; and Whitacre 25,
27G).The selective spinal anesthetic technique also contributed to this
increase in spinal anesthesia. Valia et al. (7) evaluated patient attitudes
towards regional anesthesia in Valencia, Spain. The following advantages
during surgery under regional anesthesia were referred to by 82.7% of patients:
possibility of speaking with relatives during the immediate postoperative
period (72.7%), the maintaining of consciousness during surgery (71.8%)
and the absence of pain during the immediate postoperative interval (37.3%).
Carson et al. (8) compared the use of spinal anesthesia with that of general
anesthesia in 100 young adults (aged 18-45 years) scheduled for lower body
minor surgery. The spinal anesthesia group took longer than the general
anesthesia group for surgical readiness (13±0.6 vs. 9 ±0.5
min), but much less time in recovery (57.7±3.1 vs. 72.5 ±3.6
min). Spinal anesthesia patients were quicker to drink fluids (3.4±0.3
vs. 5.1 ±0.7 hr), required less narcotic analgesia (0.6 ±1
vs. 1.2±0.2 intramuscular injections) and had a lower incidence
of vomiting (0.2±0.09 vs. 1.07±0.34). In a survey performed
at the 1993 meeting of the Society for Obstetric Anesthesia and Perinatology
(SOAP), 52% of the conference attendees reported using spinal anesthesia
as their technique of choice for elective cesarean delivery (9). Regional
anesthesia offers safe, effective and cheap anesthesia when performed by
trained personnel. The Kilimanjaro Christian Medical Center in Tanzania
(10) produces its own lidocaine and crystalloid intravenous fluids. Volatile
and intravenous anesthetic agents are often unavailable and considered
expensive. Supplies of oxygen are also unreliable. Hence, spinal and epidural
anesthesia are frequently performed for lower abdominal and lower extremity
procedures. Patients in Canada and Scotland were asked to complete a pre-operative
questionnaire examining their desire for information relating to anesthesia.
Details of dangerous complications of anesthesia and surgery were consistently
rated of low priority, with high priority going to postoperative landmarks
such as eating and drinking. Both countries rated meeting the anesthetist
before surgery as the highest priority of all (11). In the second edition
of Principles and Practice of Obstetric Analgesia and Anesthesia edited
by Bonica and McDonald (12) and published in 1995, there are 1,344 pages.
The chapter on epidural analgesia and anesthesia contains 127 pages. That
on subarachnoid block - 26 pages. On subarachnoid/epidural combination
there is only half a page with only 2 references in the chapter on cesarean
section. So, the new combined spinal-epidural anesthesia and analgesia
gained only 0.03% of the space in a book published in 1995 on the practice
of obstetric analgesia and anesthesia. This is really not its present,
neither its future... Rawal (13) mailed a questionnaire in April 1993 to
105 European anesthesiologists in 5-10 hospitals from each of the 17 European
countries. Data requested was for 1992. A total of 102 (96.2%) completed
questionnaires. Except for Ireland, combined spinal-epidural anesthesia
was used in every participating country. It was used in 53% of participating
hospitals. During 1992, 835,986 in-patient surgical procedures were performed
in the participating European hospitals, 141,444 (17%) of those procedures
were performed under central blocks (epidural,spinal, combined spinal-epidural).
A total of 5,348 combined spinal-epidural blocks were performed during
1992, which constitutes only 4% of the central blocks (spinal - 56%; epidural
- 40%; combined spinal-epidural - 4%). The commonest indication for combined
spinal-epidural block was hip replacement surgery (28.2%) followed by hysterectomy
(19%), knee surgery (14.4%), cesarean section (14%), emergency cesarean
section (13%), femur fracture in elderly patients (7.2%) and prostatectomy
(5.6%). Special combined spinal-epidural sets were used by 31% respondents;
the remaining used their own combinations of epidural needles and extra
long spinal needles. 1. Rawal N. Epidural and intrathecal opioids for postoperative
pain management in Europe - A 17-nation survey. ASRA Annual Meeting 1995:45
2. Wurm WH. Regional anesthesia and analgesia for same-day surgery in adults.
Current Opinion in Anaesthesiology 1994;7:436-440 3. Lyons G, Macdonald
R, Mikl B. Combined epidural/spinal anaesthesia for Caesarean section:
Through the needle or in separate spaces? Anaesthesia 1992;47:199-201 4.
Osborne GA, Rudkin GE. Outcome after day-care surgery in a major teaching
hospital. Anaesth Intensive Care 1993;21:822-827 5. Urmey WF, Stanton J,
Sharrock NE. Initial one-year experience of a 97.3% regional anesthesia
ambulatory surgery center. Reg Anesth 1993;18:69 6. Florio R, Sassu B,
Cianciullo A. Selective spinal technique and atraumatic needles increase
the incidence of spinal anesthesia. Acta Anaesthesiol Scand 1995;39:A432
7. Valia JC, De Andres J, Gil A, Bolinches R. Analysis of patient attitudes
towards regional anaesthesia. Int Monitor Reg Anaesth 1993:57 8. Carson
D, McLead G, Serpell M, Bannister J. Minor surgery for young adults: general
or spinal anaesthesia? Int Monitor Reg Anaesth 1993:51 9. Riley ET, Cohen
SE, Macario A, Desai JB, Ratner EF. Spinal versus epidural anesthesia for
cesarean section: A comparison of time efficiency, costs, charges, and
complications. Anesth Analg 1995;80:709-12 10. Smith J, Egan E. Regional
anaesthesia in a developing country. Int Monitor Reg Anaesth 1993:57 11.
Lonsdale M, Hutchison GL. Patient`s desire for information about anaesthesia:
Scottish and Canadian Attitudes. Anaesthesia 1991;46:410-412 12. Bonica
JJ, McDonald JS, eds. Principles and practice of obstetric analgesia and
anesthesia. 2nd ed, Williams & Wilkins, 1995 13. Rawal N. European
trends in the use of combined spinal epidural technique - A 17-nation survey.
Reg Anesth 1995;20(Suppl):162
Epidural catheter strength
A 10 cm segment of four epidural catheters to be tested was suspended
vertically from a stand, and weights were hung from it until it broke to
investigate the comparative strengths of 19 gauge epidural catheters. The
concord - Portex`s weight at break was 2,042±67 gm while that of
Kendall - 1,674 ±67 gm, Arrow (Flex Tip Plus with spiral wire reinforcement)
- 1,370±16 gm and Becton-Dickinson only 1,284±149 gm were
needed for its breakage. 1. Blum S, Sosis M. An investigation of the comparative
strengths of 19 gauge epidural catheters. Reg Anesth 1995;20(Suppl):157
Epidural catheter paresthesias
Rolbin et al. (1) reported a 24-44% incidence of transient paresthesias
during epidural catheter insertion. Juneja et al. (2) compared the incidence
of transient paresthesias among three types of epidural catheters. The
Flex Tip Plus (19 gauge; open tip; Arrow) produced only 2.16% paresthesias,
while the 20 gauge Copolymer Bullet tip (Kendall) - 15.16%, and the 20
gauge Polymide, open tip, Perifix (Braun) - 32.24%. It was concluded that
the softer tip epidural catheters like Flex Tip Plus (Arrow) were least
likely to cause transient paresthesias during epidural catheter placement.
Spriggs et al. (3) compared between Arrow`s wire reinforced epidural catheter
(Flex Tip Plus; 19 gauge; open tip) and Braun`s Perifix (18 gauge; open
tip). They found that the wire reinforced catheter was inferior than the
Perifix in its inability of insertion (8/50 vs. 0/51) and the incidence
of catheter related transient paresthesias (5/42 vs. 0/51). Huhtala et
al. (4) examined the incidence of transient radicular irritation after
spinal anesthesia with hyperbaric 5% lidocaine compared to 0.5% hyperbaric
bupivacaine and 0.5% plain bupivacaine. 10.2% of patients anesthetized
with hyperbaric lidocaine complained of radicular irritation compared to
1% of patients anesthetized with hyperbaric bupivacaine and none of the
patients in the plain bupivacaine group. 1. Rolbin SH, Hew E, Olgilvie
G. A comparison of two types of epidural catheters. Can J Anaesth 1987;34:459-461
2. Juneja M, Kargas GA, Miller DL, Perry EA, Gupta B, Garcia E, Pajel V,
Botic Z, Rigor B. Comparison of epidural catheter`s induced paresthesias
in parturients. Reg Anesth 1995;20(Suppl):152 3. Spriggs LE, Vasdev GM,
Leicht CH. Clinical evaluation of wire impregnated epidural catheters with
standard epidural catheters for labor analgesia. Reg Anesth 1995;20(Suppl):154
4. Huhtala J, Tarkkila P, Tuominen M. Transient radicular irritation after
spinal anaesthesia with hyperbaric 5% lidocaine. Acta Anaesthesiol Scand
1995;39:A426
CSEA and anticoagulation
Intraoperative anticoagulation with heparin appears relatively safe
if epidural catheters are inserted prior to anticoagulation (1,2). 1. De
Angelis J. Hazards of subdural and epidural anesthesia during anticoagulant
therapy: A case report and review. Anesth Analg 1972;51:676-679 2. Odoom
JA, Sih IL. Epidural analgesia and anticoagulant therapy. Experience with
one thousand cases of continuous epidurals. Anaesthesia 1983;38:254-259
Combined spinal-epidural analgesia in labor
Pain during the first stage of labor is attributed to uterine contractions
that contribute to dilation of the lower uterine segment and cervix. During
this stage, neural transmission of painful sensation to the neuroaxis travels
via sympathetic fibers that enter at the 10th, 11th, and 12th thoracic
and 1st lumbar spinal segments (1). These fibers synapse with ascending
and descending fibers in the dorsal horn of the spinal cord. As labor progresses
to the second stage, additional pain is produced by stretching and distention
of the vagina and perineum. This pain is more somatic in nature and is
conveyed by the pudendal nerve that arises from 2nd, 3rd, and 4th sacral
nerves (2). Interactive computer questioning of 218 delegates at the meeting
of the Society for Obstetric Anesthesiology and Perinatology in 1993 revealed
that only 4.2% clinicians did not add opioids to bupivacaine for epidural
analgesia in labour. Fentanyl and sufentanil were chosen by 97% (3). In
the UK, 30% of 272 obstetric units surveyed by Davies et al. (4) stated
that they used opioids in routine epidural analgesia for normal labor,
but only when an infusion technique was employed. Scott et al. (5) in 1980,
first reported the use in labor of "single-shot" intrathecal morphine.
Abouleish et al. (6) suggested that the use of combined spinal-epidural
analgesia in labor "avoids the requirement for setting up infusion devices,
tubing, and solutions routinely used for continuous epidural infusion techniques"
since all of their patients delivered with only the original intrathecal
dose, or a small amount of epidural local anesthetic as a supplemental
bolus. Columb et al. (7) found that the minimum local analgesic concentration
of epidural bupivacaine in labor is 0.065%. Breen et al. (8) compared two
regimes of epidural anesthesia for labor in ambulatory parturients: epidural
fentanyl bolus of 75 µg diluted to 15 ml with normal saline with
an epidural infusion of fentanyl 2.5 µg/ml at 15 ml/hr vs. epidural
bolus of bupivacaine 0.04% 15 ml, epinephrine 1.7 µg/ml and fentanyl
1.7 µg/ml, following by an infusion of this combination at 15 ml/hr.
Patients experiencing inadequate analgesia at any time were given one 10
ml bolus of the study drug. Any patient not made sufficiently comfortable
by the study drug, including the additional 10 ml bolus, was given 10 ml
of bupivacaine 0.125% with fentanyl 150 µg added, followed by an
infusion of bupivacaine 0.125% with fentanyl 2 µg/ml. 48% in the
bupivacaine-epinephrine-fentanyl group and 79% in the fentanyl group needed
these bolus augmentations. Justins et al. (9) first published in 1982 the
use of fentanyl-bupivacaine mixtures for epidural analgesia in labor. Since
the continuous infusion epidural analgesia needs supplementary top-ups
in many cases it should be termed more accurately a continuous infusion
- intermittent bolus epidural analgesia. However, intermittent low-dose
epidural injections every approximately 90 minutes will avoid the need
for the patient to be connected to an infusion set, and on the other hand
will allow the "walking epidural" due to the low dose injections at equal
times, without waiting for the analgesic effect to wear off. Enever et
al. (10) believed that "infusions rather than intermittent technique...
are safer and more effective". However, in their study of epidural infusion
of diamorphine with bupivacaine in labor 63.2% - 66.8% required top-up
injections of bupivacaine during the epidural catheter infusion technique.
Wlodarski et al. (11) found that adding 250 µg nalbuphine to a 10
µg sufentanyl in 1 ml saline mixture for the spinal injection in
the combined spinal-epidural analgesia for labor reduced significantly
the incidence of pruritus: 62% in the sufentanyl group compared to only
20% in the sufentanyl-nalbuphine group. Using an extradural mixture, in
labor, of 0.1% bupivacaine with fentanyl 30 µg in 15 ml, the initial
test dose of 0.5% bupivacaine 3 ml is unnecessary, as the single bolus
of 15 ml of the extradural mixture serves equally to detect accidental
subarachnoid injection without producing a total spinal block (12). It
is the total amount of local anesthetic drug which determines the extent
of a subarachnoid block and not its volume (13). Ewen et al. (14) have
been shown in parturient women that analgesia obtained by infusing 0.25%
bupivacaine 8 ml/hr is inferior to that obtained by giving the same mass
of drug as 0.07% bupivacaine 25 ml/hr. Eddleston et al. (15) found no advantage
to either mother or fetus in using an extradural infusion of 0.125% bupivacaine
compared with intermittent injections of 0.25% bupivacaine. In the intermittent
group, the majority of fetal decelerations (73.8%) were recorded as transient,
whereas in the infusion group 61.1% of episodes lasted in excess of 10
min. Silva and Popat (16) described a 34-year-old parturient with Harrington
rods in whom they have done a combined spinal-epidural analgesia for labor.
Using the needle-through-needle technique they injected 1 ml 0.25% bupivacaine
and 25 µg fentanyl through the spinal needle. The epidural catheter
was not tested after insertion. Two hours after the spinal injection the
patient requested a top up. 15 ml 0.1% bupivacaine with 2 µg/ml fentanyl
were injected epidurally without success. Further 10 ml of 2% lidocaine
1:200,000 epinephrine injected epidurally produced a dense motor block
in both legs but did not reduce the pain. Another combined spinal-epidural
procedure was done at the same interspace and a similar spinal dose of
bupivacaine and fentanyl again resulted in excellent pain relief for two
hours. Because of a high breech with cervical dilatation of 9 cm the patient
needed a cesarean section. However, she declined regional anesthesia and
had a cesarean delivery under general anesthesia. Sufentanil 5, 10 and
15 µg and fentanyl 25, 37.5 and 50 µg as intrathecal solutions
for labor analgesia were compared in 36 parturients using the combined
spinal-epidural analgesia. Duration of analgesia or pruritus were not affected
by drug dosage, but rather by drug choice. Both the duration of analgesia
and pruritus were longer for sufentanil than for fentanyl (17). In a review
of analgesia for labor Crowhurst (3) stated that "with the advent of `pencil-point`
spinal needles, the simpler technique of subarachnoid blockade will almost
certainly continue to supplant other methods, especially for late first
stage and second stage labour". Joos et al. (18) used a combined spinal-epidural
analgesia technique in 620 parturients. The spinal injection consisted
of 1 mg 0.5% bupivacaine, 25 µg adrenaline,and 5 µg sufentanil.
When pain returned bolus doses of 10 ml saline containing 12.5 mg bupivacaine
0.125%, 12.5 µg adrenaline and 12.5 µg sufentanil were injected.
Spinal analgesia was perfect in 94%. The mean duration of the spinal analgesia
was 134 min. All parturients were able to move perfectly both legs. Transient
pruritus occurred in 48% of women, drowsiness in 12%. The postspinal headache
rate was 0.8%. The injections were made by a 16G Tuohy epidural needle
and a 29G 113 mm Quincke spinal needle inserted through it. Caldwell et
al. (2) used the combined spinal-epidural analgesia in 26 parturients.
Subarachnoid injection consisted of morphine 0.25 mg with fentanyl 25 µg.
In cases where additional analgesia was requested, epidural analgesia was
initiated with 10 ml of bupivacaine 0.25%, followed by an infusion of bupivacaine
0.125%, with fentanyl 1 µg/ml. 76% of patients requested additional
epidural analgesia. Side effects were nausea and vomiting (50%) and pruritus
(50%). One patient developed postdural puncture headache, following unintentional
dural puncture with the 18 gauge Tuohy needle. Bonica and McDonald (19)
referred to their double-catheter technique (lumbar epidural catheter and
caudal catheter) as "the ultimate in analgesia/anesthesia for labor and
vaginal delivery, and is often referred to by anesthesiologists as the
`Rolls Royce` of obstetric analgesia and anesthesia". In comparison, the
combined spinal-epidural analgesia and anesthesia is the "Mercedes Benz"...
Hill et al. (20) compared the efficacy of intrathecal 250 µg alfentanil
and 400 µg diamorphine in combination with 0.5 ml of 0.5% bupivacaine
(2.5 mg) in the combined spinal-epidural analgesia in labor. If labour
continued beyond the duration of the subarachnoid block analgesia was maintained
with a top-up of 15 ml of 0.125% bupivacaine followed by an infusion of
0.125% bupivacaine at 8 ml/hr. Abdominal analgesia was inadequate in 8%
in the alfentanil group and in 44% in the diamorphine group. Sympathetic
block occurred in 20% of the alfentanil group and none of the diamorphine
group. 32% of the women in the alfentanil group were unable to walk after
20 min due to motor block. Transient fetal bradycardia was seen in 20%
of the alfentanil group and none of the diamorphine group. Pruritus was
common in both groups (over 90%). Arkoosh et al. (21) compared the subarachnoid
injection of fentanyl 2.5 µg with morphine 0.25 mg to sufentanil
10 µg with morphine 0.25 mg for labor analgesia using the combined
spinal-epidural analgesia. Both fentanyl and morphine and sufentanil and
morphine provided adequate labor analgesia for about 2 hours. However,
patients who received sufentanil experienced more severe pruritus. Norris
et al. (22) compared epidural versus combined spinal-epidural (CSE) technique
for maternal pain relief during labor in 1022 laboring parturients. 9.6%
of the women chose not to receive neuroaxial labor analgesia; 38% chose
epidural while 52.4% received combined spinal-epidural analgesia. The CSE
was done by a long spinal needle (27G Whitacre or 24G Sprotte) passed through
a 18G epidural needle. After withdrawing the spinal needle the epidural
needle was rotated cephalad and a 20G epidural catheter inserted through
it. In 94.4% of the CSE group the epidural and subarachnoid spaces were
successfully identified. In 4.9% of them no CSF was obtained and only epidural
analgesia was induced. There was an incidence of 0.2% of the epidural catheter
entering subarachnoid space after dural puncture with a 24G Sprotte spinal
needle. In 0.8% an accidental dural puncture occurred while rotating the
epidural needle. 1. Shnider SM, Levinson G, Ralston DH. Regional anesthesia
for labor and delivery. In: SM Shnider, G. Levinson, eds. Anesthesia for
obstetrics, 3rd ed., Baltimore, Williams & Wilkins, 1987, p.135 2.
Caldwell LE, Rosen MA, Shnider SM. Subarachnoid morphine and fentanyl for
labor analgesia: Efficacy and adverse effects. Reg Anesth 1994;19:2-8 3.
Crowhurst JA. Analgesia for labour. Curr Opin Anaesthesiol 1994;7:224-228
4. Davies M, Harrison J, Ryan T. Current practice of epidural analgesia
during normal labour. A survey of maternity units in the United Kingdom.
Anaesthesia 1993;48:63-65 5. Scott PV, Bowen FE, Cartwright P, Mohan Rao
BC, Deeley D, Wotherspoon HG, Sumrein IMA. Intrathecal morphine as sole
analgesia during labour. Br Med J 1980;278:351-353 6. Abouleish A, Abouleish
E, Camann W. Combined spinal-epidural analgesia in advanced labour. Can
J Anaesth 1994;41:575-578 7. Columb MO, Lyons G, Vail A. Estimation of
the minimum local analgesia concentration (MLAC) of epidural bupivacaine
hydrochloride in labour. International Monitor on Regional Anaesthesia
1994;A89 8. Breen TW, Shapiro T, Glass B, Foster-Payne D, Oriol NE. Epidural
anesthesia for labor in an ambulatory patient. Anesth Analg 1993;77:919-924
9. Justino DM, Francis D, Houlton PG, Reynolds F. A controlled trial of
extradural fentanyl in labour. Br J Anaesth 1982;54:409-414 10. Enever
GR, Noble HA, Kolditz D, Valentine S, Thomas TA. Epidural infusion of diamorphine
with bupivacaine in labour: A comparison with fentanyl and bupivacaine.
Anaesthesia 1991;46:169-173 11. Wlodarski JC, Tanck EN, Newman LM, Ivankovich
AD. Nalbuphine added to intrathecal sufentanyl ameliorates the pruritus
in laboring patients. Anesth Analg 1994;78:S483 12. Morgan BM, Kadim MY.
Mobile regional analgesia in labour. Br J Obstet Gynaecol 1994;101:839-841
13. Van Zundert AA, Wolf AM, Vaes L, Soetens M. High volume spinal anesthesia
with bupivacaine 0.125% for cesarean section. Anesthesiology 1988;69:998-1003
14. Ewen A, McLeod DD, MacLeod DM, Campbell A, Tunstall ME. Continuous
infusion epidural analgesia in obstetrics. A comparison of 0.08% and 0.25%
bupivacaine. Anaesthesia 1986;41:143-147 15. Eddleston JM, Maresh M, Horsman
EL, Young H, Lacey P, Anderton J. Comparison of the maternal and fetal
effects associated with intermittent or continuous infusion of extradural
analgesia. Br J Anaesth 1992;69:154-158 16. Silva TSS, Popat MT. Combined
spinal-epidural anesthesia in parturient with Harrington rods. Reg Anesth
1994;19:360 17. Gaiser R, Adams H, Cheek TG, Gutsche BB. Comparison of
three different doses of intrathecal fentanyl and sufentanyl for labor
analgesia. ASRA Annual Meeting 1995;75 18. Joos S, Servais R, Van Steenberge
A. Sequential spinal-epidural analgesia for pain relief during labour.
International Monitor on Regional Anaesthesia 1994;A88 19. Bonica JJ, McDonald
JS. Epidural analgesia and anesthesia. In: Bonica JJ, McDonald JS. eds.
Principles and Practice of Obstetric Analgesia. 2nd ed., Williams &
Williams, 1995, p.442 20. Hill DA, McAuley DM, Clarke RSJ. Randomised double
blind comparison of intrathecal alfentanil or diamorphine with bupivacaine
in a single space, needle through needle, combined spinal-epidural for
analgesia in labour. International Monitor on Regional Anaesthesia 1994;A94
21. Arkoosh VA, Sharkey SJ, Norris MC, Isaacson W, Honet JE, Leighton BL.
Subarachnoid labor analgesia: Fentanyl and morphine versus fentanyl and
morphine. Reg Anesth 1994;19:243-246 22. Norris MC, Grieco WM, Borkowski
M, Leighton BL, Arkoosh VA, Huffnagle HJ, Huffnagle S. Complications of
labor analgesia: epidural versus combined spinal epidural techniques. Anesth
Analg 1994;79:529-537
Combined spinal-epidural anesthesia for orthopedic operations
In some hospitals the combined spinal-epidural anesthesia is the method
of choice in all surgical interventions of the lower extremities. For example,
in the Endo-Clinic in Hamburg, since 1989 till 1994 there were over 13,602
cases of combined spinal-epidural anesthesia (1). Urmey et al. (2) compared
the use of 40, 60 or 80 mg isobaric lidocaine 2% injected subarachnoidally
in the needle-through-needle technique for ambulatory knee arthroscopy
in 90 patients aged 18-60 years. 24.5% of patients required separate spinal
injections due to inadequate protrusion length of the 120 mm 27G Whitacre
spinal needle through the 3 inch Weiss epidural needle. Seven patients
required epidural reinforcement doses intraoperatively. Motor recovery
onset was at 82.3±20.3 minutes in the 40 mg lidocaine 2% group,
108.2 ±25.6 - in the 60 mg and 122.8±25 in the 80 mg spinal
injection. 1. Schleinzer W, Hook D, Reibold JP, Schmalz B. Combined spinal/epidural
anaesthesia (CSE) - An appropriate procedure. Acta Anaesthesiol Scand 1995;39:A424
2. Urmey WF, Stanton J, Sharrock NE. Combined spinal-epidural (CSE) technique
to assess dose-response of isobaric lidocaine spinal anesthesia. Anesth
Analg 1993;76:S441
Combined end-multiple lateral holes (CEMLH) epidural catheter
Most of the epidural catheters used in the USA are of the single terminal
hole, while most of those used in the UK are of the three lateral holes
with a blunted end (1). A new epidural catheter was designed which is claimed
to combine the benefits of these two different types of catheters: Combined
end-multiple lateral holes epidural catheter (CEMLH). Curbelo (2) in 1947
was the first to use an epidural catheter for epidural anesthesia. It was
of the end hole type. Lee (3) in 1962 described an epidural catheter which
its "tip is non-patent and smooth, to facilitate insertion, solution enters
the space from a small opening 1 cm from the tip". Skinner (4) in 1966
described another epidural catheter with "the tip of the cannula...is blunt...and
has a hole in its end. There is a second hole, 3 mm from the distal end".
He said that "with the hole in this position, kinking is impossible with
the stresses involved in normal use". Collier and Gatt (5) described an
epidural catheter, with a closed end and three holes spaced at approximately
2, 3 and 4 mm from the smooth closed tip. They suggested that the close
spacings of the holes will eliminate the complication of multicompartment
block (epidural, spinal or intravenous), as seen with earlier multihole
epidural catheters. The CEMLH epidural catheter has 7 holes within its
1.5 cm head: One at the tip; the first 3 lateral holes are arranged circumferentially
at 1 mm from each other; the other 3 holes have a 4 mm distance from one
to the other. All the holes are within the 1.5 cm from the tip. The area
of the 6 lateral holes is the same , so the anesthetic solution stream
is the same from each hole, depending on the correct pressure elicited
upon the syringe plunger. While introducing the epidural catheter for 3
cm into the epidural space there is a proximal 1.5 cm with 7 holes and
a distal 1.5 cm which is "blind". The epidural catheter (CEMLH) has the
following possible claimed advantages: The end hole can recognize an intravascular
or intrathecal insertion of the epidural catheter tip, which a blunted
tip cannot, but an open-end catheter can; The six lateral holes spaced
at 1.5 cm from the tip allow anesthetic solution injection into the epidural
space in case that the end hole or one of the lateral holes is obstructed
by a blood clot or tissue; The chance that all the 7 holes will be blocked
is six times less than the one open-end hole and 4 times less than the
three lateral holes closed-end catheter; The CEMLH epidural catheter gives
a better distribution of the anesthetic solution due to its 7 holes, avoiding
a partial block; The CEMLH epidural catheter also afford the use of a lesser
amount of anesthetic solution to achieve an anesthetic level than the present
used catheters, due to its even distribution, without preferrence to any
side; Because of its small end hole the CEMLH catheter will give less paresthesias
than the bigger end hole catheter. The terminal hole catheter elicits more
paresthesias than the rounded closed end side hole catheter (6). Michael
et al. (7) compared between the open-end (single hole) and closed-end (three
lateral holes) epidural catheters. They found that the open-end catheters
"caused an unacceptably high incidence of unsatisfactory sensory blockade".
Collier and Gatt (5) also found the incidence of unsatisfactory blocks
with terminal hole catheter to be "unacceptably High" (32%) when compared
with the three lateral holes catheter (12%). Ward et al. (8) found that
the pressure elicited upon a lateral double-orifice epidural catheter (orifices
180 degrees opposed 5 mm and 12 mm from the closed end tip) is important
whether it will exit fluid from the proximal or the distal holes. In order
to achieve injection through the two holes at the same time they needed
to exceed the pressure of 900 torr. With a pressure of 700 torr, ejection
was only from the proximal port. If one of the three lateral holes epidural
catheter is obstructed the injection through the catheter can miss this
direction and result in partial block. If the end hole epidural catheter
is obstructed you need to replace it. Just to remind us: Before Lee (3)
described in 1962 his prepackaged epidural catheter anesthetists had employed
polyvinyl chloride tubing and nylon infant`s ureteric catheters and cut
it by themselves. Lee himself said that his epidural catheter "will also
withstand autoclaving several times without deterioration". It seems that
we have already passed the point of epidural catheter autoclaving. However,
other problems confronting us: Inadvertent intrathecal or intravascular
insertion; partial blockade; unreliability of the present used epidural
catheters with need to supplement it by a prior anesthetic solution injected
through the epidural needle, etc. 1. Collier CB, Gatt SP. Epidural catheter
for obstetrics: Terminal hole or lateral eyes? Reg Anesth 1994;19:378-385
2. Curbelo MM. Continuous peridural segmental anesthesia by means of an
ureteral catheter. Anesth Analg 1949;28:13-23 3. Lee JA. A new catheter
for continuous extradural analgesia. Anaesthesia 1962;17:248-250 4. Skinner
BS. A new epidural cannula. Can Anaesth Soc J 1966;13:622-623 5. Collier
CB, Gatt SP. A new epidural catheter: Closer eyes for safety? Anaesthesia
1993;48:803-806 6. Segal S, Eappen S, Datta S. Comparison of single-orifice
and multi-orifice epidural catheters for labor analgesia and cesarean delivery.
ASRA Annual Meeting 1995:149 7. Michael S, Richmond MN, Birks RJS. A comparison
between open-end (single hole) and closed-end (three lateral holes) epidural
catheters. Anaesthesia 1989;44:578-580 8. Ward CF, Osborne R, Benumof JL,
Saidman LJ. A hazard of double-orifice epidural catheters. Anesthesiology
1978;48:362-364
Double-hole pencil-point spinal needle
Greene (1) described in 1926 a needle with a point that is "round, tapering,
and sharp". This was the result of experiments made by him during 1923
(2) and his experience since then that brought him to the conclusion that
"postpuncture headache is caused by trauma to the spinal dura sufficient
to result in excessive leakage of cerebrospinal fluid to the point at which
the brain is left without a water cushion". His experiments demonstrated
that a greater trauma was produced by the use of a needle with a blunt
cutting point than by a needle of the same caliber with a point rounded,
tapering and sharp. He found also that it was possible to pass a small
sharp, round, tapering pointed instrument between the fibers of a spinal
dural sac, suspended and filled with water, without cutting any of them.
He performed 215 consecutive punctures with his needle, with a headache
incidence of two in the series. In many instances the puncture was done
during the noon hour, and the patient resumed his work for the remainder
of the day... Kirschner (3) in 1931 described a needle for spinal anesthesia
with an opening in the shaft just proximal to the beveled closed end. Such
a needle was recommended to aid in the more accurate control of the duration
and extent of anesthesia, since it could be manipulated to permit the injection
of solution in the stream flowing parallel to the long axis of the spinal
fluid column rather than against the side of the canal opposite puncture.
Hart and Whitacre (4) described in 1951 their pencil-point spinal needle,
known since as the Whitacre needle. Sprotte, Schedel and Pajunk (5) in
1987 modified the Whitacre needle, known since as the Sprotte needle. The
FDA approves only the use of the pencil-point spinal needle in the needle-through-needle
or the Eldor needle techniques for the combined spinal-epidural anesthesia.
However, the long orifice of 24 gauge Sprotte spinal needles may result
in failed spinal anesthetics when they are used, since this length exceeds
the 1 mm thickness of human lumbar dura (6). Sprotte has modified this
device by reducing the length of the orifice. Sosis et al. (6) compared
in vitro the 1.8 mm long laterally placed orifice of the original version
of the Sprotte spinal needle with the 1.0 mm long new Sprotte needle. They
found that the flow of water through the needle was not reduced after the
orifice length was reduced by 44%. Lipov et al.(7) examined whether the
window design of Sprotte pencil point needles leads to deformation under
lateral or axial loading conditions. They examined the 22- and 24-gauge
Sprotte, 22- and 25-gauge Whitacre and 22- and 25-gauge Quincke needles.
The force needed to bend the Sprotte needles was less than needed for the
Whitacre and Quincke needles of similar size when lateral or axial pressure
was applied. Examination of the needle tips demonstrated that the Sprotte
needles were most likely to bend at the needle window, while the Quincke
and Whitacre needles deformed at the point of clamping. They concluded
that the Sprotte needles have an inherent design weakness to lateral and
axial pressure, which may result in a greater number of needle tip deformations
upon needle insertion. The nature of this deformation may result in difficulty
in needle withdrawal and possibly fracture of the needle tip. A new pencil-point
spinal needle is described: It is named double-hole pencil-point (DHPP)
spinal needle, and is composed of a blunt ogival tip and two circular holes
opposing each other just proximal to the tip. The area of the two holes
is almost the same as of the single hole Sprotte needle`s area, which enables
more rapid CSF reflux. The anesthetic solution injection spreads through
both holes. There is a possible advantage of a more diffuse anesthetic
distribution and less anesthetic solution dosage. The DHPP spinal needle
allows anesthetic solution injection when one of the holes is obstructed
by a tissue fragment, through the opposite hole. Using the DHPP spinal
needle is like inserting two Whitacre needles in the same interspace, from
the point of view of the hole`s area. There is a possibility to avoid the
risk of needle deformation due to bending at the window, as it is the case
with the Sprotte needle. In this respect it is more like the Whitacre needle.
However, unlike the Whitacre needle there is a possibility of a two times
rapid CSF reflux, because of a double orifice area. There is also a possibility
for a more even distribution of the anesthetic solution through the opposite
holes of the DHPP spinal needle as compared to the Whitacre or Sprotte
one-sided orifice spinal needles. On account of that there is a possibilty
to reduce the anesthetic solution dosage with less untoward effects due
to a larger spinal anesthetic dose needed in the Whitacre or Sprotte spinal
needles. 1. Greene HM. Lumbar puncture and the prevention of postpuncture
headache. JAMA 1926;86:391-392 2. Greene HM. A technic to reduce the incidence
of headache following lumbar puncture in ambulatory patients with a plea
for more frequent examinations of the cerebrospinal fluids. Northwest Med
1923;22:240 3. Kirschner M. Versuche zur Herstellung einer gurtelformigen
Spinal-anasthesie. Arch Klin Chir 1931;167:755-760 4. Hart JR, Whitacre
RJ. Pencil-point needle in prevention of postspinal headache. JAMA 1951;147:657-658
5. Sprotte G, Schedel R, Pajunk H. Eine atraumatische Universalkanule fur
einzeitige Regionalanaesthesien. Reg Anaesth 1987;10:104-108 6. Sosis MB,
Braverman B, Toppses A. An in vitro evaluation of the new shorter orifice
Sprotte spinal needle. Anesth Analg 1994;78:S410 7. Lipov EG, Sosis MB,
McCarthy RJ, Ivankovich AD. Does the design of the Sprotte spinal needle
reduce the force needed to deform the tip? J Clin Anesth 1994;6:411-413
Epidural catheter test dose in the combined spinal-epidural anesthesia
The epidural test dose was first recommended by Dogliotti (1) in 1933.
He suggested a small volume of local anesthetic through the epidural needle
to insure that a subarachnoid placement had not occurred prior to injecting
the full epidural dose. Scott (2) in 1988 wrote in an editorial that "many
anaesthetists do not use (epidural test dose) unless they have serious
doubts on the correct position of the needle or catheter". Brown (3) in
the 4th edition of Miller`s textbook Anesthesia wrote that "in spite of
an adequately positioned catheter during first use of local anesthetic,
each subsequent injection should be preceded by aspiration and an epidural
test dose, since catheter migration into vessels and subarachnoid or subdural
spaces does occur." Moore (4) in his handbook on regional block advocates
the use of "2 cc of the local anesthetic solution" to be injected "at the
rate of 1 cc per 6 to 8 seconds" as an epidural catheter test dose. An
epidural test dose is considered mandatory (5). Albright (6) suggested
that the test dose should consist of 3 ml 0.5% bupivacaine with 1:200,000
epinephrine. This kind of test dose should be adequate to detect intravascular
placement as it produces a rapid increase in pulse rate. This test dose
is also adequate to detect a subarachnoid injection because a significant
motor or sensory block will occur within 5 minutes. Some authors recommend
that every top-up should be preceded by a test dose or given in fractions
(6,7). Crawford (8) in his review of 27,000 lumbar epidural blocks concluded
that "the requirements for safety are that all top ups are given in divided
doses, with an interval of approximately 5 minutes between the two increments."
The epidural catheter test dose consists of either 1 ml of hyperbaric lidocaine
with adrenaline or 2 ml of 0.5% bupivacaine with adrenaline (9). A volume
of 1.5 ml has also been recommended (10). The epidural catheter test dose
is a must maneuver, because as Moore (11) said on the epidural needle,
none of us has "an eye on the end of the needle", neither on the end of
the catheter introduced through that needle. Soresi (12) was the first
to describe the combined spinal-epidural anesthesia in 1937.He called it
"episubdural anesthesia" and thought it is "the safest procedure giving
perfect surgical anesthesia, ideal relaxation and eliminating practically
all postoperative pain and distress". Soresi first injected 7-8 ml of 20
centigrams novocain into the epidural space and then insert the spinal
needle further into the spinal space and injected there 2 ml of 10-15 centigrams
novocain. These 7-8 ml injected into the epidural space can be looked now
as the first "test dose" in the combined spinal-epidural technique. He
recommended "to inject only 7 to 8 cc of fluid in the epidural space because
large amounts of fluid will make the pressure in the epidural space positive.
This increased pressure being contrary to natural conditions is the reason
for the troubles noticed in the ordinary epidural anesthesia". Soresi also
stated that "to make episubdural anesthesia safer the anesthesiologist
must be absolutely certain of the position of the needle". Rawal (13) injected
into the subarachnoid space 1.5-2 ml 0.5% hyperbaric bupivacaine through
a 26-27G spinal needle in 24 parturients scheduled for cesarean section.
Fifteen minutes later he injected fractional doses of 5 ml 0.5% bupivacaine
through the epidural catheter (range: 5-10 ml). Myint et al. (14) published
the first case report of cardiorespiratory arrest following combined spinal-epidural
anesthesia. Using the needle-through-needle technique in a 31-year-old
parturient scheduled for cesarean section they injected into the spinal
space 2 ml 0.5% bupivacaine in 8% dextrose through 24G Sprotte needle.
Then they rotated the epidural needle 180° and introduced an epidural
catheter with three lateral holes into the epidural space. They made an
aspiration test which was negative for blood or CSF. Then they made a test
dose of 2 ml 0.5% bupivacaine with adrenaline 1:200,000 given through the
epidural catheter. A few minutes later the patient complained of some numbness
in her fingers, but her hand grip was strong and she was able to breathe
deeply and strongly on request. Upper limit of sensory block was T4 bilaterally.
At the end of the operation they have given 2.5 mg of diamorphine in 5
ml of 0.25% bupivacaine through the epidural catheter for postoperative
analgesia. Forty minutes later she complained of difficulty in breathing
which developed rapidly to respiratory and cardiac arrest. Resuscitation
started with endotracheal intubation, adrenaline 1 mg and atropine 0.6
mg i.v. Then she received two doses of naloxone 0.4 mg i.v. The patient
started breathing and regained consciousness within 2 min of the first
administration of intravenous naloxone. Her recovery was complete with
no neurological deficit. She also did not develop a postspinal headache.
Due to the masking of the epidural test dose by the previous spinal anesthetic
injection Myint et al. could not appreciate correctly the patient`s complaint
of "some numbness in her fingers". If it would occur at the first place,
i.e., the epidural catheter test dose injected before the spinal anesthetic
injection, their suspicion would certainly be of an intravascular or subarachnoid
inadvertent placement of the epidural catheter or one of its three lateral
holes. Their inability to recognize it was caused by the technique of the
needle-through-needle in which you need first to inject the anesthetic
solution into the spinal space and then to insert the epidural catheter
into the epidural space. Thoren et al.(15) used the combined spinal-epidural
technique in 21 parturients scheduled for cesarean section. Hyperbaric
bupivacaine 0.5% was injected intrathecally. Additional bupivacaine was
injected through the epidural catheter in fractionated doses. After an
initial "test dose" of 2 ml 0.5% bupivacaine, an additional 2 ml per unblocked
segment was given through the epidural catheter until a T4 level was achieved.
Kumar (16) observed that when an epidural catheter is threaded after a
spinal block was performed in the needle-through-needle technique, "a minute
quantity of clear, or slightly red-tinged fluid sometimes comes back through
the catheter". The source of this minute quantity of fluid is either CSF
or local anesthetic agent. He advocated an aspiration test before giving
the epidural medication to extend the spinal block. Spinal dura mater thickness
at the lumbar region is 0.5 mm (17). Using magnetic resonance imaging (MRI)
in 39 patients Westbrook et al. (18) found that the depth of the extradural
space at the level of T12 is 0.83 ± 0.195 cm. There are many reports
of failed aspiration tests for both subarachnoid and intravascular epidural
catheter placement (19-21). Aspiration test through an epidural needle
was suspected as a cause for dural puncture. In eight of 31 patients (25.8%)
aspiration produced CSF flow. It was not possible to say whether the aspiration
caused puncture of the dura or just revealed it, but "the suspicion remains
that aspiration of a Tuohy needle may cause dural puncture by increasing
the transdural pressure gradient" (22). In the first 1,000 epidural cases
reported by Crawford (23), of 71 dural taps, nine were with the catheter.
In his second series of 1,000, Crawford reported 33 dural taps, four of
which were caused by the catheter (24). Epidural catheter migration has
been shown to be relatively common, occurring in approximately one-third
of the patients in one study (25). Hogan (26) suggested another mechanism
for the "migration" of an epidural catheter: the membrane which separates
the lateral epidural spaces from the anterior venous confluence ruptures,
allowing local anesthetic to pour from the epidural space into the circulation.
Another mechanism of epidural catheter "migration" is rupture of subdural
bleb of local anesthetic into the CSF (27). The incidence of epidural needle/catheter
unintentional dural puncture range from 2.5% (28) to 0.6% (29) and even
0.26% (30). Recognized intravascular placement or migration of an epidural
catheter occurs in 5.2% of obstetric epidural anesthetics (31). Chadwick
et al. (32) reviewed the malpractice claims filed against anesthesiologists
in USA in 1985. There were 190 claims for care involving obstetric anesthesia
(OB) and 1,351 of claims not involving obstetric anesthesia cases. Sixty
five percent (124) of the OB claims were associated with regional anesthesia.
Of the 17 claims for newborn brain injury attributed to an anesthetic cause,
13 had regional anesthesia as the primary technique. Of the 13 associated
with regional anesthesia, 9 involved a convulsion, 8 of which appeared
due to intravascular local anesthetic injection. Convulsions were much
more common in the OB claims (10%). Eighteen of 19 convulsions occurred
in patients having epidural anesthesia. Seventeen of the convulsions appeared
to be due to local anesthetic toxic reactions. In 10 of these cases, epinephrine
containing test doses were not used; in 7 others, data were not sufficient
to determine if epinephrine-containing test doses were used or not. The
local anesthesia used in 15 cases was bupivacaine, and in 2 other cases
was not specified. Two of the convulsions appeared to be eclamptic. Eighty
three percent of the convulsions resulted in neurologic injury or death
to the mother, newborn, or both. Dain et al. (43) in 1987 distinguished
in their review on the epidural test dose in obstetrics between "what is
medically safe and what is legally safe. The authors have the impression
that in order to be `legally safe` one must perform a test dose". In conclusion,
it seems that the needle-through-needle technique for the combined spinal-epidural
anesthesia has an inherent risk because of its inability to perform properly
the epidural catheter test dosing. This can result in intravascular or
subarachnoid local anesthetic or opioid inadvertent injections. Using the
Eldor needle technique for the combined spinal-epidural anesthesia the
epidural catheter can be inserted before the spinal local anesthetic is
injected, allowing a proper epidural catheter test dosing, as it is done
in a regular epidural anesthesia. The comparison between these two techniques
(the needle-through-needle and the Eldor needle) makes the Eldor needle
technique safer from the epidural catheter test dose point of view. 1.
Dogliotti AM. Segmental peridural anesthesia. Am J Surg 1933;20:107-18
2. Scott DB. Test doses in extradural block. Br J Anaesth 1988;61:129-130
3. Brown DL. Spinal, epidural, and caudal anesthesia. In: Anesthesia, Miller
RD (ed.); Churchill Livingstone; 4th ed.; 1994;p.1525 4. Moore DC. Regional
block. Charles C. Thomas; 4th ed.; 1981;p.433 5. Shnider SM, Levinson G.
Anesthesia for cesarian section. In: Anesthesia for obstetrics; 2nd ed.;
Shnider SM, Levinson G (eds.); Baltimore: Williams and Wilkins; 1987; p.161
6. Galloon S. Test doses in extradural analgesia. Br J Anaesth 1978;50:304
7. Rees GAD, Rosen M. Test-dose in extradural analgesia. Br J Anaesth 1979;51:70-71
8. Crawford JS. Some maternal complications of epidural analgesia for labour.
Anaesthesia 1985;40:1219-1225 9. Moore DC, Batra MS. The components of
an effective test dose prior to epidural block. Anesthesiology 1981;55:693-6
10. Kumar CM, Dennison B, Panchal HI. Epidural test dose. Anaesthesia 1985;40:1023
11. Moore DC. Accidental dural puncture - who has an eye on the end of
a needle. Anaesth Intensive Care 1986;14:208 12. Soresi AL. Episubdural
anesthesia. Anesth Analg 1937;16:306-10 13. Rawal N. Single segment combined
subarachnoid and epidural block for caesarean section. Can Anaesth Soc
J 1986;33:254-5 14. Myint Y, Bailey PW, Milne BR. Cardiorespiratory arrest
following combined spinal epidural anaesthesia for caesarean section. Anaesthesia
1993;48:684-686 15. Thoren T, Holmstrom B, Rawal N, Schollin J, Lindeberg
S, Skeppner G. Sequential combined spinal epidural block versus spinal
block for cesarean section: Effects on maternal hypotension and neurobehavioral
function of the newborn. Anesth Analg 1994;78:1087-92 16. Kumar CM. More
on combined subarachnoid and epidural techniques. Anaesthesia 1986;41:90-91
17. Cheng PA. The anatomical and clinical aspects of epidural anesthesia.
Part 1. Anesth Analg 1963;42:398-406 18. Westbrook JL, Renowden SA, Carrie
LES. Study of the anatomy of the extradural region using magnetic resonance
imaging. Br J Anaesth 1993;71:495-498 19. Ravindran RS, Bond UK, Tasch
MD, Gupta CD, Luerssen TG. Prolonged neural blockade following regional
analgesia with 2-chloroprocaine. Anesth Analg 1980;59:447-51 20. Reisner
LS, Hochman BN, Plumer MH. Persistent neurologic deficit and adhesive arachnoiditis
following intrathecal 2-chloroprocaine injection. Anesth Analg 1980;59:452-4
21. Moore DC, Spierdijik J, Vankleef LD, Coleman RL, Love GF. Chloroprocaine
neurotoxicity: four additional cases. Anesth Analg 1982;61:155-9 22. Hollway
TE, Telford RJ. Observations on deliberate dural puncture with a Tuohy
needle: depth measurements. Anaesthesia 1991;46:722-724 23. Crawford JS.
Lumbar epidural block in labour: A clinical analysis. Br J Anaesth 1972;44:66-74
24. Crawford JS. The second thousand epidural blocks in obstetric hospital
prctice. Br J Anaesth 1972;44:1277-1287 25. Bishton IM, Martin PH, Vernon
JM, Liu WH. Factors influencing epidural catheter migration. Anaesthesia
1992;47:610-2 26. Hogan QH. "Migration" of an epidural catheter? Anesth
Analg 1993;76:910-911 27. Reynolds F, Speedy HM. The subdural space: the
third space to go astray. Anaesthesia 1990;45:120-3 28. Dawkins CJM. An
analysis of the complications of extradural and caudal block. Anaesthesia
1969;24:554 29. Tanaka K, Watanabe R, Harada T, Dan K. Extensive application
of epidural anesthesia and analgesia in a university hospital: incidence
of complications related to technique. Reg Anesth 1993;18:34-38 30. Macdonald
R. Unintentional dural puncture. Anaesthesia 1988;43:705 31. Kenepp NB,
Gutsche BB. Inadvertent intravascular injections during lumbar epidural
anesthesia. Anesthesiology 1981;54:172-173 32. Chadwick HS, Posner K, Caplan
RA, Ward RJ, Cheney FW. A comparison of obstetric and nonobstetric anesthesia
malpractice claims. Anesthesiology 1991;74:242-249 33. Dain SL, Rolbin
SH, Hew EM. The epidural test dose in obstetrics; is it necessary? Can
J Anaesth 1987;34:601-5
Spinal and epidural opioid analgesia
Epidural bolus injection of opioid, morphine and fentanyl, can produce
good analgesia in doses of 2-4 mg and 0.1-0.2 mg, respectively (1). In
animal studies, it has been demonstrated that intrathecal or epidural coadministration
of opioid and local anesthetics produced synergistic analgesia (2-5). The
use of continuous epidural opioid infusions may obviate the need for redosing,
but it may obligate the patient to receive more opioid than is required
(6) and increase the risk of respiratory depression (7). Drug dose is the
important determinant of efficacy, rather than concentration or volume
(8). Torda et al. (9) found that in patients who had undergone major abdominal
surgery, analgesia after thoracic extradural injection of fentanyl 50 µg
did not differ significantly from analgesia after 0.5% bupivacaine 10 ml,
or the fentanyl-bupivacaine mixtures. Bupivacaine alone caused a greater
decrease in arterial pressure and a higher incidence of hypotension than
fentanyl or the fentanyl-bupivacaine mixtures. Badner et al. (10,11) reported
that after abdominal, thoracic or knee replacement surgery, there was no
advantage in using a mixture of 0.1% bupivacaine with fentanyl 10 µg/ml
compared with fentanyl alone by continuous extradural infusion. Rudolph
Matas (12), on November 10, 1899, was the first in the U.S. to apply the
subarachnoid anesthesia. Matas may have been the first to inject morphine
into the subarachnoid space (13). Moreno et al. (14) described three patients
treated by CSF rechange after total spinal block caused by mistaken overdosage
of local anesthetic in the subarachnoid space (two after epidural and one
after paravertebral blocks). In all three patients clinical features of
total spinal block appeared with severe hypotension, respiratory depression
and loss of consciousness. After crystalloid perfusion and epinephrine
administration, CSF rechange was performed. A 22G spinal needle was introduced
in a cervical space in two patients and in a lumbar space in one patient.
Repeated removal of 5 ml of CSF was followed by replacement of an equal
volume of saline solution up to a volume of 50 ml. In less than 5 minutes
all three patients recovered normal blood tension, spontaneous respiration
and consciousness, while spontaneous movements of the four limbs were achieved
between 20-30 minutes. The method was also used for the treatment of subarachnoid
morphine overdose (15). Addition of 20 µg of fentanyl to plain lidocaine
5% in dextrose (50 mg) spinal anesthesia improve duration of sensory anesthesia
without prolonging recovery of motor function or time to micturition (16).
Sosis et al. (17) have shown that staphylococcus aureus and candida albicans
continue to survive 51 hr after inoculation of fentanyl/bupivacaine mixtures.
The fraction of the lumbar epidural dose found in CSF after epidural sufentanil
75 µg, diluted in 10 ml saline, was 2.7%. The time to peak CSF sufentanil
concentration was 0.76±0.50 hr in the lumbar area and 2.1±1.4
hr in the thoracic area (18). The availability to CSF of epidural morphine
is 2% and of epidural pethidine - 10% (19). Spinal anesthesia has been
achieved with meperidine as a sole agent (20). Meperidine has also been
used for spinal analgesia during labor and delivery (21) because it provides
sensory anesthesia with a weak motor block (22). 1. De Castro J, Meynadier
J, Zenz M. Regional opioid analgesia. Dordrecht: Kluwer Academic Publishers,
1991, p. 198-200 2. Akerman B, Arwestrom E, Post C. Local anesthetics potentiate
spinal morphine antinociception. Anesth Analg 1988;67:943-948 3. Penning
JP, Yaksh TL. Interaction of intrathecal morphine with bupivacaine and
lidocaine in the rat. Anesthesiology 1992;77:1186-1200 4. Maves TJ, Gebhart
GF. Antinociceptive synergy between intrathecal morphine and lidocaine
during visceral and somatic nociception in the rat. Anesthesiology 1992;76:91-99
5. Kaneko M, Saito Y, Kirihara Y, Kosaka Y. Effects of epidural morphine
and lidocaine on somatic and visceral pain. Neuroscience Abstracts 1991;17:294
6. Marlowe S, Engstrom R, White PF. Epidural patient-controlled analgesia
(PCA): an alternative to continuous epidural infusions. Pain 1989;37:97-101
7. Boudreault D, Brasseur L, Samii K, Lemoing J. Comparison of continuous
epidural bupivacaine infusion plus either continuous epidural infusion
or patient-controlled epidural injection of fentanyl for postoperative
analgesia. Anesth Analg 1991;73:132-137 8. Laveaux MMD, Hasenbos MAWM,
Harbers JBM, Liem T. Thoracic epidural bupivacaine plus sufentanyl: High
concentration/low volume versus low concentration/high volume. Regional
Anaesthesia 1993;18:39-43 9. Torda TA, Hann P, Mills G, DeLeon G, Persman
D. Comparison of extradural fentanyl, bupivacaine and two fentanyl-bupivacaine
mixtures for pain relief after abdominal surgery. Br J Anaesth 1995;74:35-40
10. Badner NH, Komar WE. Bupivacaine 0.1% does not improve postoperative
epidural fentanyl analgesia after abdominal or thoracic surgery. Can Anaesth
Soc J 1992;39:330-336 11. Badner NH, Reimer EJ, Komar WE, Moote CA. Low-dose
bupivacaine does not improve postoperative epidural fentanyl analgesia
in orthopedic patients. Anesth Analg 1991;72:337-341 12. Matas R. Local
and regional anesthesia with cocaine and other analgesic drugs, including
the subarachnoid method, as applied in general surgical practice. Phil
Med J 1900;6:820-843 13. Vandam LD. On the origins of intrathecal anesthesia.
International Anesthesiology Clinics 1989;27:2-7 14. Moreno LA, Sinche
M, Balust J, Izquierdo E, De Jose Mana B, Sala X, Galard JJ, Nalda MA.
Total spinal block (TSB) treated by means of cerebrospinal fluid rechange
(CSFR). International Monitor on Regional Anesthesia 1993;68 15. Kaiser
KG, Bainton CR. Treatment of intrathecal morphine overdose by aspiration
of cerebrospinal fluid. Anesth Analg 1987;66:475-477 16. Liu S, Carpenter
RL, Neal JM, Pollock JE, Gerancher JC. Effects of addition of 20 µg
of fentanyl to lidocaine spinal anesthesia. Reg Anesth 1995;20:S112 17.
Sosis M, Braverman B, Ivankovich A. Growth of Candida albicans and staphylococcus
aureus in Fentanyl/Bupivacaine mixtures for epidural administration. Society
of Obstetric Anesthesia and Perinatology (SOAP), 25th Annual Meeting, 1993:92
18. Hansdottir V, Woestenborghs R, Nordberg G. The cerebrospinal fluid
and plasma pharmacokinetics of sufentanil after thoracic or lumbar epidural
administration. Anesth Analg 1995;80:724-729 19. Nordberg G, Hansdottir
V, Bondesson U, Boreus LO, Mellstrand T, Hedner T. CSF and plasma pharmacokinetics
of pethidine and norpethidine in man after epidural and intrathecal administration
of pethidine. Eur J Clin Pharmacol 1988;34:625-631 20. Famewo CE, Naguib
M. Spinal anaesthesia with meperidine as the sole agent. Can Anaesth Soc
J 1985;5:533-537 21. Swayze C, Sherman JH, Walker EB. Efficacy of subarachnoid
meperidine for labor analgesia. Reg Anesth 1991;16:309-313 22. Sangarlankarn
S, Klaewtanong V, Jonglerttrakool P, Khankaew V. Meperidine as a sole anesthetic
agent: A comparison with lidocaine-glucose. Anesth Analg 1987;66:235-240
The choice of the anesthesiologists
Gantt et al. (1) evaluated whether anesthesiologists will still prefer
spinal or epidural anesthesia over general anesthesia after they will experience
these regional techniques. Twelve anesthesiologists underwent two procedures
(spinal and epidural anesthesia) on the same day. All but one anesthesiologist
(91.6%) did not change their preference for regional over general anesthesia.
In a survey among 558 Canadian surgeons they have been asked which anesthesia
they would choose for themselves for a hernia repair. The results were:
local - 38%; general - 30%; epidural - 15%; spinal - 10%; other - 6% (2).
The choice was somewhat surprising, because surgeons rarely perform local
anesthesia on patients for hernia repair. It was also interesting to note
that the the method of anesthesia selected by the surgeons for themselves
was not necessarily the method they would choose for their patients. 1.
Gantt R, Beardsley D, Lindsey J, Setzer V, Stevens RA. Subjective preferences
of twelve anesthesiologists undergoing two major neuroaxial blockades:
spinal and epidural. Anesthesiology 1994;81:A990 2. Klassen N, Grace M,
Finucane BT. Surgeons` attitudes towards regional anesthesia: a Canadian
perspective. ASRA Annual Meeting 1995;107
Epidural catheter malposition
In a survey (1) conducted in 218 obstetric units in the UK in 1993,
99% of the units resited the epidural catheter following an inadvertent
dural tap. One percent inserted the epidural catheter into the subarachnoid
space to provide continuous spinal analgesia. There are many reports of
failed aspiration tests for both subarachnoid and intravascular catheter
placement (2-4). Epidural catheter test dose is a must maneuver, because
as Moore (5) said on the epidural needle, none of us has "an eye on the
end of the needle", neither on the end of the catheter introduced through
that needle. The incidence of inadvertent epidural catheter intravascular
cannulation range from 5.6% (6) to 4.8% (7) and even 0.67% (8). Brown (9),
in the 4th edition of Miller`s Anesthesia wrote that "in spite of an adequately
positioned catheter during first use of local anesthetic, each subsequent
injection should be preceded by aspiration and an epidural test dose, since
catheter migration into vessels and subarachnoid or subdural spaces does
occur". Campbell et al. (10) evaluated the spinal injection of 2.5 mg bupivacaine,
10 µg sufentanil and 10 µg sufentanil plus 2.5 mg bupivacaine
in 52 nulliparous patients using the needle-through-needle technique in
the combined spinal-epidural anesthesia. After spinal anesthetic injection
the 25G spinal needle was removed and the 20G epidural catheter inserted
but not tested. CSF was not obtained in 7.7% (4/52) of the patients who
subsequently had a functioning epidural catheter. 4.2% (2/48) of the epidural
catheters required replacement. Rathmell et al. (11) evaluated in 8 healthy
volunteers whether premedication with nalbuphine 0.15 mg/Kg IV has an effect
on the ability to detect auditory or taste symptoms of IV local anesthetic
injection (1.5 mg/Kg 2% chloroprocaine). They found that nalbuphine sedation
does not interfere with the detection of intravascular epidural catheters
when 2% chloroprocaine is used as a test dose. Cantelo and Walsh (12) described
a case in which an epidural catheter was inserted at the T12-L1 interspace
after an inadvertent dural puncture occurred at the L1-2 interspace. Aspiration
tests revealed 0.2-0.3 ml of CSF, which leaked from the subarachnoid space
into the epidural space. Failure to detect inadvertent intravenous injection
of a local anesthetic with epinephrine can result in cardiac arrest (13)
during general anesthesia. In the elderly (14,15) or in patients with á-adrenergic
blockade (16), systolic blood pressure changes were reported to be more
reliable than heart rate changes. Tanaka et al. (17) gave 3 ml of 1.5%
lidocaine with epinephrine (1:200,000) IV to 15 patients anesthetized with
1% end-tidal isoflurane and nitrous oxide. 5 of 15 patients developed heart
rate increments smaller than 20 beats/min. However, all patients exhibited
systolic blood pressure increases more than 15 mmHg. They concluded that
the systolic blood pressure criterion should be used to diagnose suspected
intravascular migration of the epidural catheter during combined spinal-epidural
anesthesia. Crawford (18) in his review of 27,000 lumbar epidural blocks
concluded that "the requirements for safety are that all top ups are given
in divided dose, with an interval of approximately 5 minutes between two
increments". The inadvertent intravenous administration of local anesthetic
during "epidural" injection was classified by Crawford as a "potentially
life threatening complication" (18). Scott and Hibbard (19) collated 108
nonfatal complications from more than 500,000 obstetric epidurals in the
UK from 1982 to 1986 inclusive. One out of three cardiac arrests and 21
convulsions were associated with inadvertent intravascular injection. Michels
et al. (20) found that the use of 1 mg/Kg lignocaine as a test dose would
result in a significantly higher sensitivity of subjective symptoms for
detecting intravascular injection than the use of 0.5 mg/Kg (95% vs. 50%).
The incidence of epidural needle/catheter unintentional dural puncture
range from 2.5% (21) to 0.6% (8) and even 0.26% (22). 1. Sajjad T, Ryan
TDR. Current management of inadvertent dural taps occurring during the
siting of epidurals for pain relief in labour: A survey of maternity units
in the United Kingdom. Anaesthesia 1995;50:156-161 2. Ravindran RS, Bond
UK, Tasch MD, Gupta CD, Luerssen TG. Prolonged neural blockade following
regional analgesia with 2-chloroprocaine. Anesth Analg 1980;59:447-51 3.
Reisner LS, Hochman BN, Plumer MH. Persistent neurologic deficit and adhesive
arachnoiditis following intrathecal 2-chloroprocaine injection. Anesth
Analg 1980;59:452-4 4. Moore DC, Spierdijik J, Vankleef JD, Coleman RL,
Love GF. Chloroprocaine neurotoxicity: four additional cases. Anesth Analg
1982;61:155-9 5. Moore DC. Accidental dural puncture - who has an eye on
the end of a needle. Anaesth Intensive Care 1986;14:208 6. Jaucot J. Paramedian
approach of the peridural space in obstetrics. Acta Anaesthesiol Belg 1986;37:187
7. Kenepp NB, Gutsche BB. Inadvertent intravascular injections during lumbar
epidural anesthesia. Anesthesiology 1981;54:172-173 8. Tanaka K, Watanabe
R, Harada T, Dan K. Extensive application of epidural anesthesia and analgesia
in a university hospital: incidence of complications related to technique.
Reg Anesth 1993;18:34-38 9. Brown DL. Spinal, epidural, and caudal anesthesia.
In: Anesthesia; Miller RD (ed.); Churchill Livingstone; 4th ed.; 1994;p.1525
10. Campbell DC, Camann WR, Datta S. Combined spinal-epidural for labor
analgesia: Comparison of intrathecal sufentanil vs bupivacaine vs sufentanil
plus bupivacaine. Anesthesiology 1994;81:A1145 11. Rathmell JP, Viscomi
CM, Roth J, Aladjem E, Williams J. Detection of intravascular epidural
catheters using 2-chloroprocaine injection: influence of dose and nalbuphine
premedication. Anesthesiology 1994;81:A971 12. Cantelo RA, Walsh GR. Aspiration
of cerebrospinal fluid - not always a dural tap. Anaesthesia 1993;48:452
13. Marx GF. Cardiotoxicity of local anesthetics - the plot thickens. Anesthesiology
1984;60:3-5 14. Kahn RL, Quinn TJ. Blood pressure, not heart rate, as a
marker of intravascular injection of epinephrine in an epidural test dose.
Reg Anesth 1991;16:292-5 15. Vestal RE, Wood AJJ, Shand DG. Reduced á-adrenoceptor
sensitivity in the elderly. Clin Pharmacol Ther 1979;26:181-6 16. Guinard
JP, Mulroy MF, Carpenter RL, Knopes KD. Test doses: optimal epinephrine
content with and without acute beta-adrenergic blockade. Anesthesiology
1990;73:386-92 17. Tanaka M, Yamamoto S, Ashimura H, Iwai M, Matsumiya
N. Efficacy of an epidural test dose in adult patients anesthetized with
isoflurane: Lidocaine containing 15 µg epinephrine reliably increases
arterial blood pressure, but not heart rate. Anesth Analg 1995;80:310-4
18. Crawford JS. Some maternal complications of epidural analgesia for
labour. Anaesthesia 1985;40:1219-1225 19. Scott DB, Hibbard BM. Serious
non-fatal complications associated with extradural block in obstetric practice.
Br J Anaesth 1991;64:537-41 20. Michels AMJ, Lyons G, Hopkins PM. Lignocaine
test dose to detect intravenous injection. Anaesthesia 1995;50:211-213
21. Dawkins CJM. An analysis of the complications of extradural and caudal
block. Anaesthesia 1969;24:554-563 22. Macdonald R. Unintentional dural
puncture. Anaesthesia 1988;43:705
Woolley and Roe case
On October 13, 1947, two incidents occurred which resulted in one of
the most famous of all medicolegal actions as far as the speciality of
anesthesia was concerned. Two patients, Cecil Roe and Albert Woolley who
were on the same operative list for relatively minor surgical procedures,
developed permanent, painful, spastic paraparesis following spinal anesthesia
with hypobaric 1:1500 cinchocaine (nupercaine; dibucaine) administered
by the same anesthetist. Both patients sued the hospital and the anesthetist
and the case came to court in October 1953 and lasted 11 days. This case
had a profound effect on the practice of spinal anesthesia, as anesthetists
were fearful of producing permanent neurological damage and the technique,
in the UK, was probably retarded by 20-25 years (1). Noble and Murray (2)
in a review of 78,746 spinal anesthetics in Canada, found no permanent
neurological sequelae. Similarly, Moore and Bridenbaugh (3) surveyed 12,386
and Dripps and Vandam (4) - 10,098 spinal anesthetics, and did not find
evidence of permanent neurological deficits. In an editorial published
in 1975 on spinal anesthesia Scott and Thorburn (5) wrote that "it has
been virtually ignored in the last 20 years for several reasons, including
the introduction of muscle relaxants. Since the Woolley and Roe cases,
reported in 1954, in which two patients developed painful and permanent
paraplegia following spinal anaesthesia, the use of the technique in the
United Kingdom has been confined to a few enthusiasts". 1. Morgan M. The
Woolley and Roe case. Anaesthesia 1995;50:162-173 2. Noble AB, Murray JJ.
A review of the complications of spinal anaesthesia with experience in
Canadian teaching hospitals from 1959-1969. Can Anaesth Soc J 1971;18:5-?????
3. Moore DC, Bridenbaugh LD, Bagdi PA, et al. Present status of spinal
(subarachnoid) and epidural (peridural) block: a comparison of the two
technics. Anesth Analg 1968;47:40-9 4. Dripps RD, Vandam LD. Long term
follow-up of patients who received 10,098 spinal anesthetics. JAMA 1954;156:1486-1491
5. Scott DB, Thorburn JT. Spinal anaesthesia. Br J Anaesth 1975;47:421-2
Anesthetic costs
US cost of local anesthetic drugs are much cheaper than those of general
anesthetics. For example, bupivacaine 0.5% 30 ml - $1.24; lidocaine 1%
30 ml - $0.35; fentanyl 100 µg - 0.30 compared to midazolam 5 mg
- $7.27; atracurium 100 mg - $39.17; propofol 200 mg - $9.63. Inhalational
anesthetics also cost much more: Isoflurane 100 ml -$70.75; halothane 250
ml - $14.89 (1). For total hip or knee replacement, the anesthesia related
drug costs for a spinal anesthetic are approximately one half that for
a general anesthetic (2). 1. Cooper JO. The relative costs of anesthesia
drugs in New Zealand versus the United States. Anesth Analg 1995;80:850-851
2. Bowe EA, Brill VL, Baysinger CL, Brown KL, Longston GM, Chillag KJ.
Anesthesia drug costs for total joint replacement: Spinal versus general
anesthesia. ASRA Annual Meeting 1995;21
From the skin to the spinal-epidural spaces
The distribution of distance from the skin to the epidural space in
obstetric patients (n=2,123) was: < 3 cm - 0.3%; 3 to < 4 cm - 15%;
4 to < 5 cm - 47.3%; 5 to < 6 cm - 28.6%; 6 to < 7 cm - 6.9%;
7 to < 8 cm - 1.4%; and > 8 cm - 0.5% (1). Barbara l. Leighton (2) described
her model for initial instruction in epidural catheterization technique...
the banana. The banana represents the skin, subcutaneous tissue and the
ligamentum flavum. "An average banana can be used for 30 attempts before
it becomes mushy". Unripe bananas need less frequent replacement. In addition,
an average banana`s width (3 cm) is only slightly less than the distance
from the skin to the epidural space in the average patient (4 cm) (3).
This model does not represent the vertebrae; however, bony anatomy can
be learned from a skeleton. The mean value of the distance from skin to
the epidural space in term parturients is influenced by the patient`s position
during epidural needle placement. It is 4.44 ± 0.82 cm in the sitting
position and 5.03 ± 1.05 cm in the lateral position (1). Spinal
dura mater thickness at the lumbar region is 0.5 mm (4). Using magnetic
resonance imaging (MRI) of 39 patients Westbrook et al. (5) found that
the depth of the extradural space at the level of T12 is 0.83±0.195
cm. Cerebrospinal fluid is formed at the rate of 400 ml/day (6). The average
adult has a total of 120 to 150 ml of fluid, of which only 20 to 35 ml
are in the spinal portion of the subarachnoid space. In parturients, this
volume in the spinal canal is decreased (7). Valsalva (8), in 1682, was
the first to remark on the CSF when he cut open the spine of a dog and
noticed the liquid "which in all its aspects resembles that which is found
in the joints". Meme et al. (9) using an epiduroscope could visualize the
pulsation of the dura synchronized to heart rate. The human dura mater
shows its fibers neither longitudinally nor parallel directed. It has thin
collagen fibers and thick elastic ones with wavy characteristics, grouped
in ribbons or sheets (10). 1. Hamza J, Smida M, Benhamou D, Cohen SE. Parturient`s
posture during epidural puncture affects the distance from skin to epidural
space. J Clin Anesth 1995;7:1-4 2. Leighton BL. A greengrocer`s model of
the epidural space. Anesthesiology 1989;70:368-9 3. Cousins MJ. Epidural
neural blockade. In: Neural blockade in clinical anesthesia and management
of pain. Cousins MJ, Bridenbaugh PO (eds.); Philadelphia; JB Lippincott,
1980:pp. 184-5 4. Cheng PA. The anatomical and clinical aspects of epidural
anesthesia. Part 1. Anesth Analg 1963;42;398-406 5. Westbrook JL, Renowden
SA, Carrie LES. Study of the anatomy of the extradural region using magnetic
resonance imaging. Br J Anaesth 1993;71:495-498 6. Franksson C, Gordh R.
Headache after spinal anesthesia and a technic for lessening its frequency.
Acta Chir Scand 1946;94:443-454 7. McDonald JS, Mandalfino DA. Subarachnoid
block. In: Bonica JJ, McDonald JS, eds. Principles and practice of obstetric
analgesia and anesthesia. 2nd ed., Williams & Wilkins, 1995;pp.479-480
8. Viets HR. Domenico Cotugno: his description of the cerebrospinal fluid.
Bull Inst Hist Med 1935;3:701-720 9. Meme E, Amici M, Ricci L, Merletti
F. Epidural space: anatomical living view. International Monitor on Regional
Anaesthesia 1993;96 10. Reina MA, Lopez A, Escriu MN, Del Cano MC, Cascales
MR, Delgado MP. Structure of human duramater by a scanning electron microscopy.
International monitor on Regional Anaesthesia 1994;A71
Myint case
Myint et al. (1) published the first case report of cardiorespiratory
arrest following combined spinal-epidural anesthesia. using the needle-through-needle
technique in a 31 year old parturient scheduled for cesarean section they
injected 2 ml 0.5% bupivacaine in 8% dextrose through 24G Sprotte needle
into the spinal space. Then they rotated the epidural needle 180° and
introduced an epidural catheter with three lateral holes into the epidural
space. They made an aspiration test which was negative for blood or CSF.
Then they made a test dose of 2 ml 0.5% bupivacaine with adrenaline 1:200,000
given through the epidural catheter. A few minutes later the patient complained
of some numbness in her fingers, but her hand grip was strong and she was
able to breath deeply and strongly on request. Upper limit of sensory block
was T4 bilaterally. At the end of the operation they have given 2.5 mg
of diamorphine in 5 ml of 0.25% bupivacaine through the epidural catheter
for postoperative analgesia. Forty minutes later she complained of difficulty
in breathing which developed rapidly to respiratory and cardiac arrest.
Resuscitation started with endotracheal intubation, adrenaline 1 mg and
atropine 0.6 mg IV. Then she received two doses of naloxone 0.4 mg IV.
She started breathing and regained consciousness within 2 min of the first
administration of intravenous naloxone. The patient recovered completely
with no neurological deficit and did not develop a postspinal headache.
Due to the masking of the epidural test dose by the previous spinal anesthetic
injection Myint et al. could not appreciate correctly the patient`s complaint
of "some numbness in her fingers". If it occurred at the first place, i.e.,
the epidural catheter test dose before the spinal anesthetic injection,
their suspicion would certainly be of an intravascular or subarachnoid
inadvertent placement of the epidural catheter or one of its 3 lateral
holes. Their inability to recognize it is blamed upon the technique of
the needle-through-needle in which you have first to inject the anesthetic
solution into the spinal space and then to insert the epidural catheter
into the epidural space. It is in contrast to the Eldor needle technique
in which the epidural catheter is first inserted allowing a proper test
dose, and then the spinal anesthetic is injected through the spinal needle
introduced through its spinal conduit. 1. Myint Y, Bailey PW, Milne BR.
Cardiorespiratory arrest following combined spinal epidural anaesthesia
for caesarean section. Anaesthesia 1993;48:684-686
Spinal needles
Slow flowback of CSF through 25 and 26-gauge spinal needles may, particularly
in inexperienced hands, lead to repeated unrecognized dural puncture and
this may contribute to post dural puncture headache. In 1968, Brandus (1)
examined 22G spinal needles and identified tissue fragments ("cores") in
75% of needles in which the stylet was not removed and CSF not seen. The
cores (skin or epidural threads) were absent when CSF was identified and
local anesthetic injected. Campbell et al. (2) compared the coring effect
between the 25G Quincke and 25G Whitacre spinal needles. Tissue fragments
were identified in 80% of the Quincke needles compared to 41% of the Whitacre
needles in which the stylet was not removed and CSF not seen, and in one
of the 25G Quincke needles in which CSF was identified and local anesthetic
injected. All tissue fragments were fat tissue. Westbrook et al. (3) compared
the force required for dural puncture with different spinal needles and
subsequent leakage of cerebrospinal fluid using an in vitro model of a
bovine dura. They found that the pencil-point needles required significantly
more force to pierce the dura than the Quincke needle of the same external
diameter. For example, using the B-D 25G Quincke needle the puncture was
0.04±0.01 Kg force, while using the B-D Whitacre needle it was three
times more - 0.12±0.02 Kg force. The CSF flow through the Quincke
needle was almost twice than that of the Whitacre needle (8.30±.9
vs 4.30±.9). This lesser leak of CSF of the pencil-point needle
compared to the Quincke needle, confirms its superiority in reducing the
incidence of post dural puncture headache. In a meta-analysis of 450 articles
published from January 1966 till December 1993 Halpern and Preston (4)
found a reduction in the incidence of postdural puncture headache when
noncutting spinal needles rather than cutting needles were used and when
a small spinal needle was used compared with a large needle of the same
type. There was no difference in the incidence of failure of spinal anesthesia
or the incidence of back pain between the noncutting and the cutting spinal
needles. Garcia et al. (5) found a significantly higher unsuccessful dural
puncture or inadequate sensory block while using 27G Whitacre needle as
compared to 25G Whitacre needle (10% vs 2%). Anderson et al. (6) used either
25G Whitacre or 27G Quincke spinal needles to induce combined spinal-epidural
labor analgesia. They were able to obtain CSF in only 28 of 37 patients
(75.6%) when using the Whitacre needle but in all of 13 patients in whom
they used the Quincke-point needle. McLeod et al. (7) described two 25G
Whitacre needles which tips resembled "concorde nose" after it struck bone
while introduced at the L3-4 interspace. Using the needle-through-needle
technique Pedraza et al. (8) found that after dural puncture with 26G Whitacre
spinal needle there were 0.11 ml CSF refluxed through the epidural needle
within 2 minutes, while with the 24G Sprotte needle there were 0.30 ml
of CSF. Using the needle-through-needle technique Joshi and McCarroll (9)
encountered difficulties to feel the spinal needle puncturing the dura.
"This could be due to the fact that the spinal needle has to brush the
curved bevel of the Tuohy needle". Turner and Shaw (10) found an increased
incidence of paresthesias (16.6%) while using the long Whitacre spinal
needles through the epidural needles in the combined spinal epidural anesthesia
for cesarean section. They postulated its long nose cone as an explanation
("before cerebrospinal fluid is evident, these needles have to be passed
further through the dura"). Injection of local anesthetics at the first
appearance of fluid at the hubs of spinal needles with long orifices (Sprotte,
Quincke, Diamond point) may result in failed spinal anesthesia due to leakage
into the epidural space. In that regard the shorter orifice spinal needle
(Whitacre) is preferred (11). Failed or incomplete spinal block with Sprotte
needles varies between 1.6% and 11.5% (12,13). This could possibly be related
to the larger length of the orifice compared to the dura. Since the thickness
of the dura is from 0.5 to almost 2.0 mm (14), and the length of the orifice
of 22 gauge Sprotte needle is 2 mm and that of the 24 gauge Sprotte is
1.4 mm, it is possible that CSF aspiration can occur while, on injection,
some of the local anesthetic escapes through that part of the orifice outside
the dura (15). Coring of the epidermis by a spinal needle with tissue deposition
and proliferation in the subarachnoid space is a presumed etiology for
iatrogenic intraspinal epidermoid tumors. These tumors have been reported
as a late complication of lumbar puncture (16,1). 1. Brandus V. The spinal
needle as a carrier of foreign material. Can Anaesth Soc J 1968;15:197-201
2. Campbell DC, Douglas J, Taylor G. Do the newer spinal needles reduce
"coring"? Anesthesiology 1993;79:A478 3. Westbrook JL, Uncles DR, Sitzman
BT, Carrie LES. Comparison of the force required for dural puncture with
different spinal needles and subsequent leakage of cerebrospinal fluid.
Anesth Analg 1994;79:769-72 4. Halpern S, Preston R. Postdural puncture
headache and spinal needle design. Anesthesiology 1994;81:1376-1383 5.
Garcia J, Arilla MC, Sierra P, Castillo J, Pares N, Escolano F, Castano
J. Spinal anaesthesia with 25G and 27G Whitacre spinal needles in patients
under 60 years of age. International Monitor on Regional Anaesthesia 1993;23
6. Anderson M, D`Angelo R, Philip J, Hood DD, Eisenach JC. Intrathecal
sufentanil compared to epidural bupivacaine for labor analgesia. Anesthesiology
1993;79:A970 7. McLeod GA, Carson D, Bannister J. "Concorde nose" in Whitacre
spinal needles. Br J Anaesth 1993;70:593 8. Pedraza I, Riobo MI, Alvarez
J. Collection of CSF using a combined spinal epidural needle as an indication
of a duramater hole spinal puncture. International Monitor on Regional
Anaesthesia 1994;A96 9. Joshi GP, McCarroll SM. Evaluation of combined
spinal-epidural anesthesia using two different techniques. Reg Anesth 1994;19:169-174
10. Turner MA, Shaw M. Atraumatic spinal needles. Anaesthesia 1993;48:452
11. Sayeed YG, Sosis MB, Braverman B, Ivankovich AD. An in vitro investigation
of the relationship between spinal needle design and failed spinal anesthetics.
Reg Anesth 1993;18:S85 12. Brettner J, Wresch KP, Klose R. Does a pencil-shaped
spinal needle offer advantages for spinal anesthesia? Reg Anaesth 1990;13:124-128
13. Crone LL, Vogel W. Failed spinal anesthesia with the Sprotte needle.
Anesthesiology 1991;75:717 14. Dittman M, Schafer HG, Ulrich J, Bond-Taylor
W. Anatomical re-evaluation of lumbar dura mater with regard to postspinal
headache: Effect of dural puncture. Anaesthesia 1988;43:635-7 15. Ackerman
W, Cases-Cristobal V, Juneja M, Rigor BM. Sprotte needle for caesarean
section. Anaesthesia 1991;46:230 16. Gardner DJ, O`Gorman AM, Blundell
JE. Interspinal epidermoid tumor: late complication of lumbar puncture.
Can Med J 1987;141:233-235
Meningitis post combined spinal-epidural anesthesia
Harding et al. (1) reported on two cases of meningitis which developed
after combined spinal-extradural procedures for obstetric analgesia. The
first case was thought to be caused by aseptic or chemical meningitis and
the second was a case of bacterial meningitis in a patient who also received
an extradural blood patch. 1. Harding SA, Collis RE, Morgan BM. Meningitis
after combined spinal-extradural anaesthesia in obstetrics. Br J Anaesth
1994;73:545-547
Preemptive analgesia and combined spinal-epidural anesthesia
Shir et al. (1) compared three groups of patients undergoing radical
prostatectomy with general, epidural or combined epidural and general anesthesia.
Preemptive analgesia was observed only with epidural anesthesia, because
this type of anesthesia allows for even minor discomfort to be noticed
and treated during surgery. They concluded that "complete intraoperative
blockade of afferent signals to the CNS is fundamental in decreasing postoperative
pain". 1. Shir Y, Raja SN, Frank SM. The effect of epidural versus general
anesthesia on postoperative pain and analgesic requirements in patients
undergoing radical prostatectomy. Anesthesiology 1994;80:49-56
Sympathetic innervation and CSEA
Sympathetic innervation to the sinoatrial node exits from the spinal
cord between T1 and T4 (1,2). Sympathetic block below these segments results
in arterial and venous vasodilation in the lower extremities and reflex
compensatory increased sympathetic activity above the block (1). Blocks
reaching the T1-4 segments would then interrupt the sympathetic flow to
the heart. Parasympathetic innervation to the heart, on the other hand,
originates in the brainstem, travels via the vagus nerve and should not
be blocked, even during high levels of spinal anesthesia (1). The adrenal
medulla, which is the only known source of plasma epinephrine, receives
its sympathetic innervation from preganglionic fibers having their cell
bodies in spinal segments T6 through L2 (3). For many years, anesthesiologists
have assumed that, when local anesthetic is given to produce a sensory
or motor block, blockade of preganglionic sympathetic fibers would be present
(4). In vivo investigations of spinal (5,6) and epidural (7,8) anesthesia
have concluded that sympathetic denervation is present during sensory and
motor centroneuraxis block and that the level of sympathetic block exceeds
the level of sensory block by at least two dermatome segments. However,
these conclusions are based on a loss of cold sensation (5,9), an increase
in skin temperature (6) or thermography (4). However, studies evaluating
sympathetic blockade by monitoring skin conductance responses (10,11) have
reported that spinal anesthesia (upper level of sensory analgesia T4-T6)
produced an incomplete sympathectomy of the lower extremity. Stevens et
al. (12) evaluated ten subjects who underwent both spinal and epidural
anesthesia with plain lidocaine on the same day with complete recovery
between blocks. Before and 30 min after local anesthetic injection, a cold
pressor test (immersion of an hand up to the wrist into an ice-water bucket
(4°C) for 120 sec) was performed. Conduction block attenuated the increase
in response to cold pressor test only in mean arterial pressure (spinal
and epidural) and cardiac index (spinal only). Neither spinal nor epidural
anesthesia blocked the increase in heart rate, norepinephrine or epinephrine
to cold pressor test. Despite a more complete motor block during spinal
anesthesia, spinal anesthesia did not produce a more complete sympathectomy
than epidural anesthesia. The myocardium and the coronary vasculature are
densely innervated by sympathetic fibers. Sympathetic tone in the coronary
circulation both at rest and during exercise may improve the matching of
coronary blood flow and myocardial oxygen demand (13). In patients with
coronary artery disease, however, there is evidence for a nonbeneficial
sympathetic influence as this matching capability is disturbed during sympathetic
stimulation (14-18). In patients with severe coronary artery disease, cardiac
sympathetic block with high thoracic epidural anesthesia increases coronary
artery stenotic diameter at rest (15), improves global as well as regional
left ventricular wall motility, and increases left ventricular ejection
fraction during exercise stress tests (19). Furthermore, in patients with
severe coronary artery disease and unstable angina refractory to maximal
medical therapy, thoracic epidural anesthesia offers efficient pain relief
(20), and decreases determinants of myocardial oxygen demand - heart rate,
preload and afterload during myocardial ischemia (14). It also seems to
"stabilize" patients with unstable angina (20,21). Thoracic epidural anesthesia
may beneficially affect the collateral flow during ischemia. It was observed
by Klassen et al. (22) that thoracic epidural anesthesia reduced the coronary
vascular resistance 20%-25% for collateral flow into the ischemic myocardium.
1. Greene NM. Physiology of spinal anesthesia. 3rd ed. Baltimore: Williams
& Wilkins, 1981 2. Lefkowitz RJ, Hoffman BB, Taylor P. Neurohumoral
transmission: the autonomic and somatic motor nervous system. In: Gilman
AG, Rall TW, Nies AS, Taylor P, eds. Goodman and Gilman`s The Pharmacologic
basis of therapeutics. 8th ed. New York: Pergamon Press, 1990:84-121 3.
Bonica JJ. Autonomic innervation of the viscera in relation to nerve block.
Anesthesiology 1968;29:793-813 4. Greene NM, Brull SJ. Physiology of spinal
anesthesia. 4th ed. Baltimore, Williams and Wilkins, 1993, pp. 21-40 5.
Greene NM. The area of differential spinal block during spinal anesthesia
with hyperbaric tetracaine. Anesthesiology 1958;19:45-50 6. Chamberlain
DP, Chamberlain BDL. Changes in skin temperature of the trunk and their
relationship to sympathetic blockade during spinal anesthesia. Anesthesiology
1986;65:139-145 7. Brull SJ, Greene NM. Zones of differential sensory block
during extradural anaesthesia. Br J Anaesth 1991;66:651-655 8. Hopf HB,
Weissbach B, Peters J. High segmental thoracic epidural anesthesia diminishes
sympathetic outflow to the legs despite restriction of sensory block to
the upper thorax. Anesthesiology 1990;73:882-889 9. Gibbons JD. Non-parametric
methods for quantitative analysis. 2nd ed. Columbus, American, 1988 10.
Bengtsson M, Loefstroem JB, Malmqvist LA. Skin conductance responses during
spinal anesthesia. Acta Anaesthesiol Scand 1985;29:67-71 11. Malmqvist
LA, Bengtsson M, Bjoernsson G, Jordfeldt L, Loefstroem JB. Sympathetic
activity and hemodynamic variables during spinal analgesia in man. Acta
Anaesthesiol Scand 1987;31:467-473 12. Stevens RA, Beardsley D, White JL,
Kao TC, Gantt R, Holman S. Does spinal anesthesia result in a more complete
sympathetic block than that from epidural anesthesia? Anesthesiology 1995;82:877-883
13. feigl E. Coronary physiology. Physiol Rev 1983;63:1-205 14. Blomberg
S, Emanuelsson H, Ricksten S-E. Thoracic epidural anesthesia and central
hemodynamics in patients with unstable angina pectoris. Anesth Analg 1989;69:558-62
15. Blomberg S, Emanuelsson H, Kvist H, Lamm C, Ponten J, Waagstein F,
Ricksten SE. Effects of thoracic epidural anesthesia on coronary arteries
and arterioles in patients with coronary artery disease. Anesthesiology
1990;73:840-7 16. Chierchia S, Lazzari M, Simonetti I, Maseri A. Hemodynamic
monitoring in angina at rest. Herz 1980;5:189-98 17. Heusch G, Deussen
A. The effects of cardiac sympathetic nerve stimulation on perfusion of
stenotic coronary arteries in the dog. Cir Res 1983;53:8-15 18. Heusch
G, Deussen A, Thamer V. Cardiac sympathetic nerve activity and progressive
vasoconstriction distal to coronary stenoses: feed-back aggravation of
myocardial ischemia. J Auton Nerv Syst 1985;13:311-26 19. Kock M, Blomberg
S, Emanuelsson H, Lomsky M, Stromblad SO, Ricksten SE. Thoracic epidural
anesthesia improves global and regional left ventricular function during
stress-induced myocardial ischemia in patients with coronary artery disease.
Anesth Analg 1990;71:625-30 20. Blomberg S, Curelaru I, Emanuelsson H,
et al. Thoracic epidural anaesthesia in patients with unstable angina pectoris.
Eur Heart J 1989;10:437-44 21. Blomberg SG. Long-term home self-treatment
with high thoracic epidural anesthesia in patients with severe coronary
artery disease. Anesth Analg 1994;79:413-21 22. Klassen G, Bramwell R,
Bromage P, Zborowska-Sluis D. Effect of acute sympathectomy by epidural
anesthesia on the canine coronary circulation. Anesthesiology 1980;52:8-15
The politics of anesthesiology
Bridenbaugh (1) in his 1994 Gaston Labat Award Lecture recalled "visiting
our congressman in the late 1980`s when we were fighting against legislation
that proposed the radiology, anesthesiology, and pathology specialities
should be reimbursed by the hospital and not our patients. In spite of
our rational and logical protests, the congressman reminded us that our
groups had little impact on the voting public. His comment was `All of
your group`s patients are either in the dark, asleep, or dead`". 1. Bridenbaugh
PO. Anesthesiology and pain management: Medical practice or perception.
Reg Anesth 1994;19:301-306
Preconclusion
John Selden was an English historian, jurist, antiquary and statesman.
He lived between 1584 and 1654. In 1689 was published a collection of his
sayings entitled: Table talk. One of them is as follows: "Preachers say,
Do as I say, not as I do. But if the physician had the same disease upon
him that I have, and he should bid me do one thing, and himself do quite
another, could I believe him?"